(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a plenary session, and a presentation by Dr. Todd Morgan discussing the AUA guidelines for salvage therapy for prostate cancer. Dr. Morgan notes that a prior guideline “Adjuvant and Salvage Radiotherapy After Prostatectomy: AUA/ASTRO Guideline” was published in 2013. Several key statements from this guideline were as follows:
- Consider restaging evaluation at the time of biochemical recurrence (CT/bone scan)
- Offer salvage therapy to patients with biochemical recurrence, the earlier the better
- Inform patients about the side effects of salvage therapy
- “Given the methodological weaknesses of this literature, it is not possible to provide guidance regarding the use of ADT in conjunction with radiotherapy”
As such, based on the vast changes in imaging and management over the last decade, there was a necessity to provide a brand-new salvage therapy guideline. Key questions asked by the panel for the new guideline were as follows: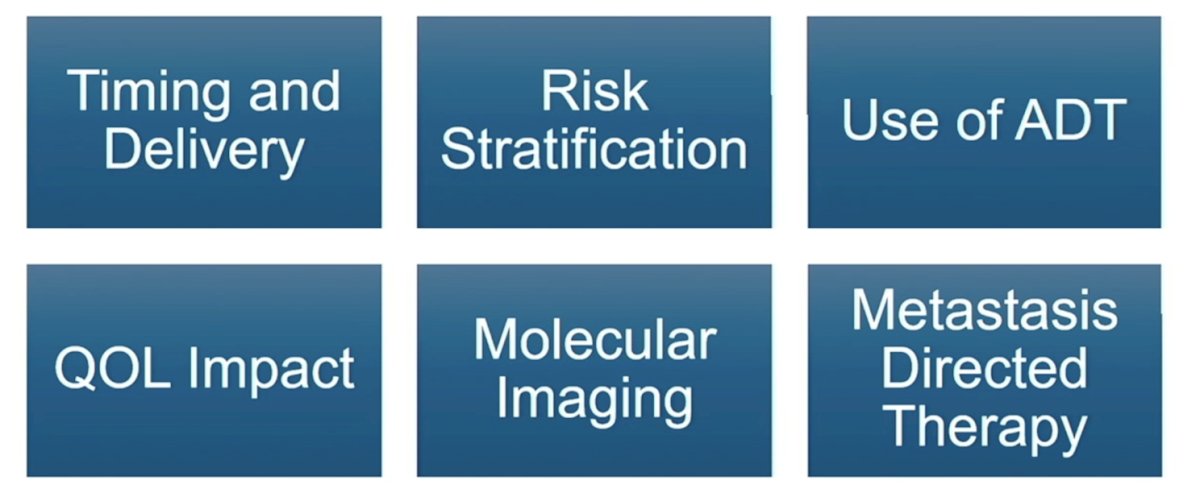
The guideline development overview included: planning, followed by a literature search, followed by study selection, followed by data extraction and quality assessment, followed by evidence interpretation, and finally recommendations. Recommendations were based on evidence from a systematic review, with some key questions being dropped if there was insufficient evidence. Each working group developed recommendations for their key questions, and recommendations were refined and finalized by the entire panel. Following this, peer review was undertaken followed by board review and approval.
The first 12 statements of this new guideline were related to treatment decision-making at the time of suspected biochemical recurrence after primary radical prostatectomy:
- Clinicians should inform patients that salvage radiation for a detectable PSA after radical prostatectomy is more effective when given at lower levels of PSA. (Strong Recommendation; Evidence Level: Grade B)
- For patients with a detectable PSA after radical prostatectomy in whom salvage radiation therapy is being considered, clinicians should provide salvage radiation when the PSA is ≤0.5 ng/mL. (Moderate Recommendation; Evidence Level: Grade B)
- For patients with a detectable PSA after radical prostatectomy who are at high risk for clinical progression, clinicians may offer salvage radiation when PSA values are <0.2 ng/mL. (Conditional Recommendation; Evidence Level: Grade C)
- Clinicians should inform patients that salvage radiation after radical prostatectomy poses inherent risks to urinary control, erectile function, and bowel function. These risks must be considered in the context of the risks posed by recurrent cancer along with patient life expectancy, comorbidities, and preferences to facilitate a shared decision-making approach to management. (Clinical Principle)
- Clinicians should use prognostic factors (e.g., PSA doubling time, Gleason Grade Group, pathologic stage, surgical margin status, validated post-prostatectomy genomic classifier, and/or PET imaging results) to counsel patients with a detectable PSA about their risk of clinical progression. (Moderate Recommendation; Evidence Level: Grade B)
The following table highlights high-risk features in the setting of biochemical recurrence to be considered for patient counseling and management: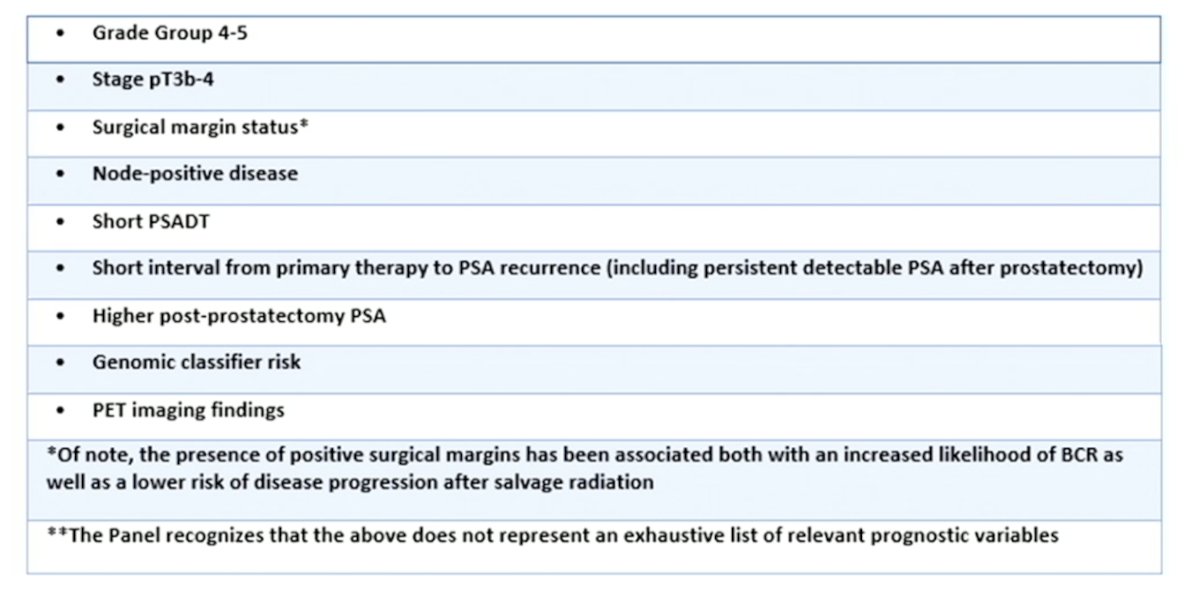
- Clinicians may obtain ultrasensitive PSA following radical prostatectomy in patients who are at high risk of recurrence and in whom salvage radiation therapy would be considered. (Expert Opinion)
- For patients who do not meet the AUA definition of biochemical recurrence after radical prostatectomy (PSA ≥0.2 ng/mL) yet have a detectable ultrasensitive PSA, clinicians should confirm a rising trend in PSA before proceeding with therapy. (Expert Opinion)
- In patients with a biochemical recurrence after local therapy, clinicians may obtain a PSMA-PET in lieu of conventional imaging or after negative conventional imaging for further evaluation of clinical recurrence. (Conditional Recommendation; Evidence Level: Grade C)
- For patients with biochemical recurrence following radical prostatectomy in whom salvage radiation is being considered, the clinician should perform next-generation molecular PET imaging. (Moderate Recommendation; Evidence Level: Grade C)
- In patients with biochemical recurrence following radical prostatectomy with PET/CT positive pelvic nodal disease, the clinician should incorporate treatment of these positive findings in the radiation plan. (Moderate Recommendation; Evidence Level: Grade C)
- In patients with biochemical recurrence, clinicians may obtain a pelvic MRI in addition to a PET/CT for evaluation of local recurrence. (Conditional Recommendation; Evidence Level: Grade C)
- In a patient with a biochemical recurrence following radical prostatectomy, clinicians should not withhold salvage prostate bed radiation therapy in the setting of a negative PET/CT. (Expert Opinion)
- Clinicians should offer ADT in addition to salvage radiation therapy for patients with biochemical recurrence following radical prostatectomy and any high-risk features (e.g., higher post-prostatectomy PSA such as PSA ≥0.7ng/mL, Gleason Grade Group 4 to 5, PSA doubling time ≤6months, persistently detectable post-operative PSA, seminal vesicle involvement). (Moderate Recommendation; Evidence Level: Grade B)
- For patients with biochemical recurrence following radical prostatectomy without any high-risk features, clinicians may offer radiation alone. (Conditional Recommendation; Evidence Level: Grade C)
- Clinicians should discuss treatment side effects and the impact of medical comorbidities when patients are being considered for ADT (as well as duration) with salvage radiation therapy, utilizing a shared decision-making approach. (Clinical Principle)
- For patients with pN1 disease being treated with postoperative radiation therapy, clinicians should include ADT rather than treating with radiation therapy alone. (Clinical Principle)
- When providing ADT to patients undergoing salvage radiation therapy, clinicians should provide a minimum of four to six months of hormonal therapy. (Clinical Principle)
- For patients with high-risk features, clinicians may extend ADT to 18 to 24 months. (Expert Opinion)
- In patients with biochemical recurrence following radical prostatectomy undergoing salvage radiation therapy with ADT, clinicians may use expanded radiation fields that include the regional lymph nodes. (Conditional Recommendation; Evidence Level: Grade B)
- Clinicians should discuss with patients that including treatment of regional lymph nodes with salvage radiation therapy may increase the risk of side effects, particularly in the short term, compared to prostate bed radiation therapy alone. (Moderate Recommendation; Evidence Level: Grade A)
- Clinicians should not recommend the addition of docetaxel in patients undergoing salvage radiation therapy and ADT. (Strong Recommendation; Evidence Level: Grade B)
- For pN0 patients, clinicians should recommend the use of intensified androgen receptor suppression with salvage radiation therapy only within a clinical trial setting. (Clinical Principle)
- For patients with biochemical recurrence following primary radiation therapy or ablative therapy who have no evidence of metastatic disease and are candidates for local salvage therapy, clinicians should perform a prostate biopsy to evaluate for local recurrence. (Clinical Principle)
- In patients with a biopsy-documented prostate cancer recurrence after primary radiation therapy who are candidates for salvage local therapy, clinicians should offer radical prostatectomy, cryoablation, high-intensity focused ultrasound (HIFU), or re-irradiation as part of a shared decision-making approach. (Moderate Recommendation; Evidence Level: Grade C)
- In patients for whom salvage local therapy is being considered following focal ablation, clinicians should offer whole gland treatment by radical prostatectomy or radiation therapy. (Expert Opinion)
- In patients with pelvic nodal recurrence following primary radical prostatectomy, clinicians should offer ADT plus salvage radiation therapy to the prostate bed and pelvic lymph nodes. (Expert Opinion)
- In patients with pelvic nodal recurrence following primary radiation therapy who did not receive prior pelvic nodal radiation therapy, clinicians should offer salvage pelvic nodal radiation therapy plus ADT. (Expert Opinion)
- Clinicians may offer salvage pelvic lymphadenectomy for patients with evidence of pelvic lymph node recurrence after radical prostatectomy or radiation therapy; however, these patients should be counseled regarding the uncertain oncologic benefit of surgery in this setting. (Conditional Recommendation; Evidence Level: Grade C)
- In patients with evidence of regional or metastatic oligo recurrence following primary therapy (radical prostatectomy or radiation therapy), clinicians may perform stereotactic ablative radiotherapy metastasis-directed therapy but should consider the risk of toxicity versus benefits. (Conditional Recommendation; Evidence Level: Grade C)
- In patients with biochemical recurrence who have non-regional disease seen on PET/CT but no visible disease on conventional imaging, clinicians may omit salvage radiation therapy to the prostate bed and should discuss the uncertain role of systemic therapy in this setting. (Expert Opinion)
Dr. Morgan concluded by highlighting several next steps for the AUA guidelines committee:
- Continued refinement to adjuvant systemic therapy with radiotherapy intensification and de-intensification
- Improved understanding of how PSMA PET should be used to change treatment decisions in the biochemical recurrence setting
- Incorporating EMBARK: intensified androgen receptor suppression in very high-risk biochemical recurrence/nmHSPC (Advanced Prostate Cancer Guidelines)
Presented by: Todd Morgan, MD, Urological Surgeon, University of Michigan, Ann Arbor, MI
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.
Related content: Optimizing Salvage Radiation Therapy in Prostate Cancer: New AUA/ASTRO/SUO Guideline - Todd Morgan


