(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a session on prostate cancer staging and a presentation by Dr. Rashid Sayyid discussing PSMA PET/CT-detected mesorectal nodal metastasis in biochemically recurrent prostate cancer patients.
One novel observation from PSMA-PET/CT based imaging is the detection of mesorectal lymph node metastases, which has been described in small series of prostate cancer patients with biochemical recurrence. Importantly, mesorectal lymph nodes fall outside the canonical lymphatic drainage zone of the prostate, and, accordingly, are not routinely included in pelvic lymph node dissection or external beam radiotherapy elective nodal irradiation volumes. As such, identification of mesorectal lymph node metastases may have important treatment implications in both the pre-and post-treatment settings, particularly for metastasis-directed therapy.
In the era of conventional imaging, clinical manifestation of lymph node metastases in this area is rare, even among patients with high-volume metastatic disease. As such, the etiology of these prostate cancer-involved mesorectal lymph nodes, as well as their clinical significance, remain unclear. The objective of this work presented by Dr. Sayyid and colleagues was to determine the prevalence and clinical predictors of mesorectal lymph node metastases in prostate cancer patients undergoing a PSMA-PET/CT scan in the setting of biochemical failure.1
This analysis was a cross-sectional analysis of all prostate cancer patients with biochemical failure following radical prostatectomy or radiotherapy who underwent an 18F-DCFPyL-PSMA-PET/CT at The Princess Margaret Cancer Centre between December 2018 and February 2021. Biochemical failure was defined using the American Urologic Association and Phoenix criteria for patients undergoing radical prostatectomy and radiotherapy, respectively. The study patients were prospectively enrolled in the PSMA-PET for Recurrent Prostate Cancer (PREP) Ontario provincial registry. Lesions with PSMA scores ≥2 were considered positive for prostate cancer involvement (PROMISE classification).2 The primary outcome was the frequency of positive mesorectal lymph nodes. The secondary objective was to evaluate demographic, oncologic, and iatrogenic (i.e. surgical manipulation) predictors of positive mesorectal lymph nodes. Analysis was stratified by primary treatment modality (radical prostatectomy versus pelvic radiotherapy). Finally, predictors of mesorectal lymph node metastasis were evaluated using univariable and multivariable logistic regression analyses.
This cohort consisted of 686 patients, with the primary treatment modality being a radical prostatectomy in 528 patients (77.0%) and radiotherapy in 158 (23.0%) patients. The median serum PSA level was 1.15 ng/ml, and the median time from primary treatment to PSMA-PET/CT scan was 5.4 years (IQR 2.5-9.7). The baseline characteristics of these patients are as follows: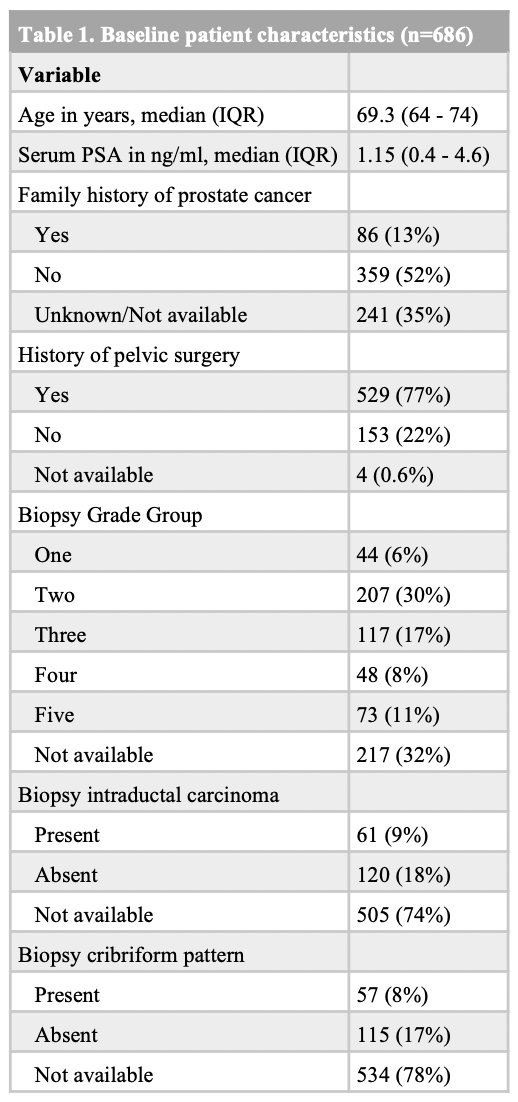
The pathologic outcomes of radical prostatectomy patients are as follows: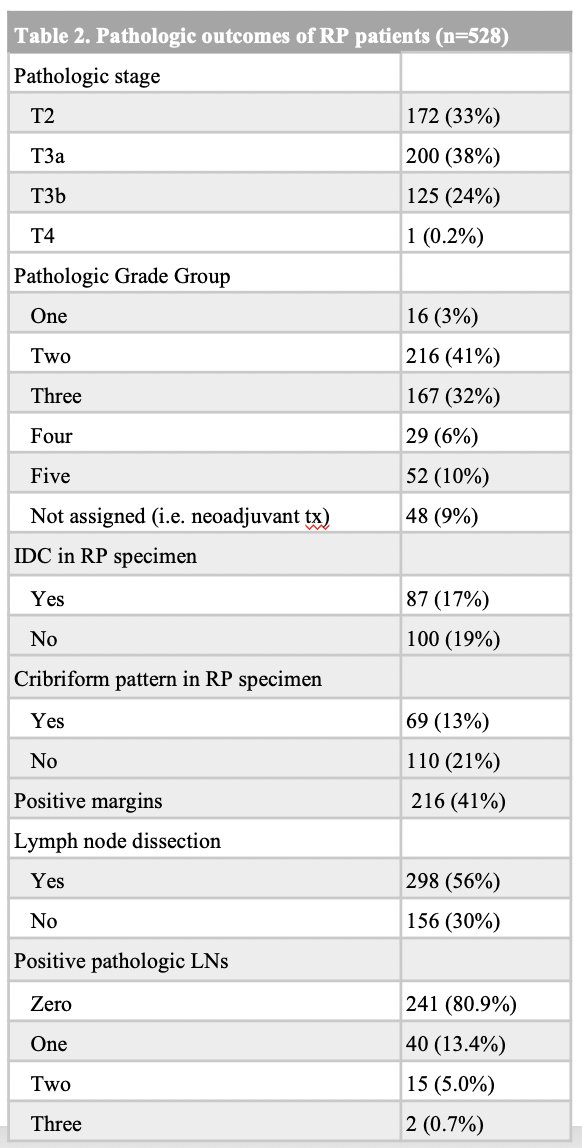
Overall, 384 patients (56.0%) had a positive scan, and 78 patients (11.3%) had mesorectal lymph node metastasis. This included a similar number of patients for those undergoing radical prostatectomy (11.1%) and radiotherapy (12.0%; p = 0.77), with a median number of positive mesorectal lymph nodes of 1 (IQR: 1-1). There were 48/78 (61.5%) of patients having mesorectal lymph node involvement as the only site of metastasis. Of the remaining 30 patients, 27 had concurrent nodal metastasis, and only three patients had concurrent non-nodal metastasis. There were 10/78 mesorectal lymph node metastasis detected on the CT component. On multivariable analysis, presence of pT3b disease (OR 4.31, 95% CI 1.44-14.2, p=0.011) was significantly associated with increased odds of mesorectal lymph node metastasis, whereas surgical factors (radical prostatectomy versus radiotherapy; performance/extent of pelvic nodal dissection), surgical margin positivity, and Gleason Grade were not associated with mesorectal lymph node metastasis: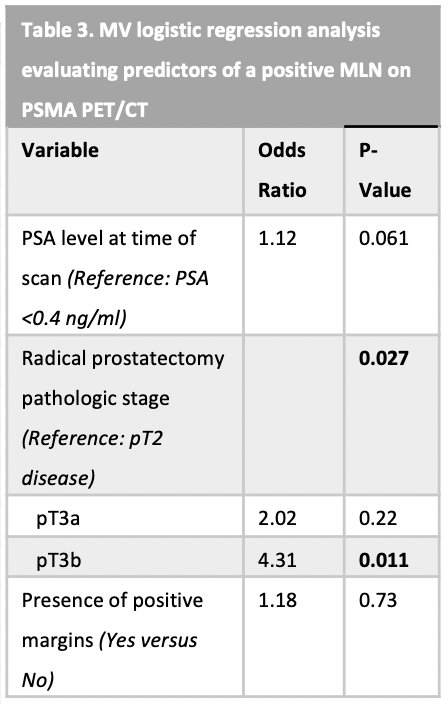
Dr. Sayyid concluded his presentation discussing PSMA PET/CT-detected mesorectal nodal metastasis in biochemically recurrent prostate cancer patients with the following take-home points:
- Approximately 11% of prostate cancer patients with biochemical failure undergoing an 18F-DCFPyL-PET/CT scan have mesorectal lymph node metastasis, with presence of pT3b disease associated with a 4.31-fold significantly increased odds of mesorectal lymph node metastasis
- These findings suggest alternate drainage routes for prostate cancer cells, either via alternate lymphatic drainage from the seminal vesicles themselves or secondary to direct extension from posteriorly located tumors invading the seminal vesicles
- The incidence of mesorectal nodal metastasis was similar for patients undergoing a radical prostatectomy or radiation therapy, and surgical factors were not significantly associated with the odds of mesorectal lymph node metastasis, suggesting that this is not an iatrogenic phenomenon
- Further work is needed to define the prognosis of mesorectal lymph node-positive patients compared to classic metastatic sites (ie. pelvic lymph nodes, bone, visceral disease)
Presented by: Rashid K. Sayyid, Urologic Oncology Fellow, Division of Urology, University of Toronto, Toronto, Ontario
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.
References:
- Morris MJ, Rowe SP, Gorin MA, et al. Diagnostic Performance of 18F-DCFPyL-PET/CT in Men with Biochemically Recurrent Prostate Cancer: Results from the CONDOR Phase III, Multicenter Study. Clin Cancer Res. 2021 Jul 1;27(13):3674-3682.
- Eiber M, Herrmann K, Calais J, et al. Prostate Cancer Molecular Imaging Standardized Evaluation (PROMISE): Proposed miTNM Classification for the Interpretation of PSMA-Ligand PET/CT. J Nucl Med 2018;59(3):469-478.


