(UroToday.com) During the COVID-19 pandemic, the rapid expansion of telemedicine brought virtual care delivery into the policy spotlight, particularly as a potential tool for addressing health equity. A study presented by Dr. Khalid Alkhatib from the University of Pennsylvania at the 2024 American Urological Association Annual Meeting, focused on how telemedicine has been utilized among cancer patients and survivors specifically focusing on prostate cancer.
Dr. Alkhatib began by reviewing the study hypothesis – given the expanded access from the widespread use of virtual care, the use of telehealth could reduce racial and ethnic disparities in prostate cancer care compared to other oncological conditions. This assumption was grounded in the backdrop of the pandemic’s public health emergency, which accelerated the integration of telehealth into routine care. Although the public health emergency has since ended, healthcare providers have advocated for the permnanent codification of telehealth expansion to maintain improved access.
The study team conducted a cross-sectional analysis of the National Health Interview Survey conducted from July 2020 to December 2021, which was chosen to represent the peak of the COVID-19 pandemic cases. Dr. Alkhatib emphasized that the study focused on two specific survey questions to identify cancer patients and survivors who used telemedicine services, identifying patients with a cancer diagnosis and those who had received virtual care. The analysis included a complex-weighted multivariable Poisson regression, adjusted for over ten demographic variables including cancer type, immunocompromised status, and socioeconomic factors.
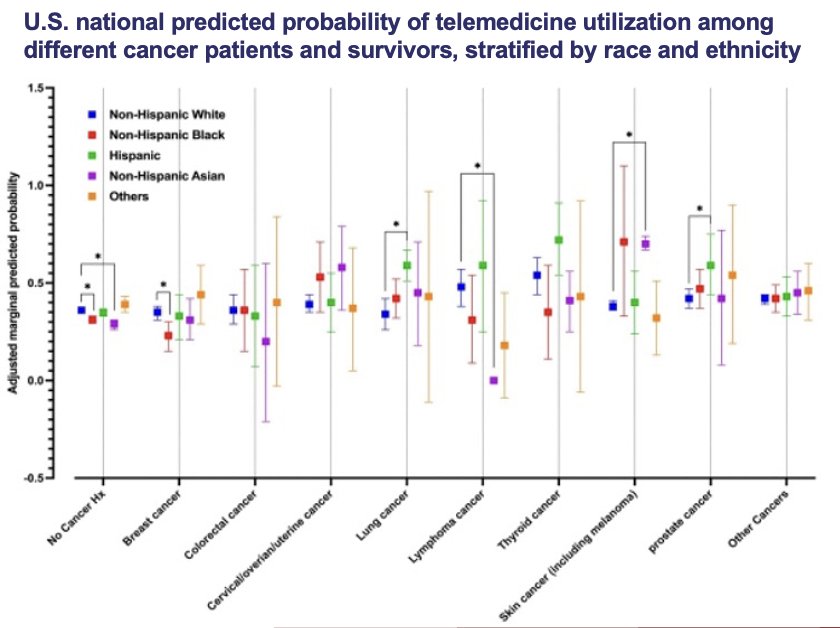
Study findings indicated that prostate cancer independently predicted higher telemedicine receipt with a relative risk (RR) of 1.28. However, disparities were noted, as Non-Hispanic Blacks (NHB) were less likely to receive telemedicine compared to Non-Hispanic Whites (NHW), with a significant interaction between race/ethnicity and cancer type. Before adjusting for this interaction, NHB were less likely to receive telemedicine. Post-adjustment, no significant disparities were found between NHB and NHW in prostate cancer telemedicine receipt, contrary to other cancer types and those with no cancer history.
As telehealth flexibility waivers are set to expire by the end of 2024, Dr. Alkhatib reinforced the urgency to establish permanent telemedicine reimbursement parity is underscored by this study. He added that study limitations include the absence of detailed patient- and provider-level variables that could explain why disparities decrease with telehealth receipt and the quality of interactions between patients and providers. He concluded by stating that the study adds crucial evidence to the discourse on health equity, indicating that targeted telemedicine interventions can potentially equalize access to care for diverse racial and ethnic groups, particularly in prostate cancer treatment.
Presented by: Khalid Alkhatib, MD, MMSc, University of Pennsylvania, Philadelphia, PA
Written by: Ruchika Talwar, MD, Urologic Oncology Fellow, Vanderbilt University Medical Center, during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


