(UroToday.com) During the American Urological Association 2024 Annual Meeting in San Antonio, Texas, Dr. Apoorv Dhir from the University of Michigan delivered a podium presentation focused on the determinants of financial toxicity in patients with urologic cancer. Financial toxicity refers to the economic strain experienced by patients due to medical expenses, which can significantly impact their quality of life and access to care. This cross-sectional investigation aimed to explore the pervasive issue of financial toxicity that many patients face following a diagnosis of urologic cancer.
Dr. Dhir began his presentation with the example of a 67-year-old male diagnosed with metastatic prostate cancer. As his treatment with ADT (Androgen Deprivation Therapy) and abiraterone commenced, the compounded burdens of severe fatigue, depression, and financial strain from novel treatments led to his premature retirement. Residing 80 miles from the cancer center, the logistical challenges and opportunity costs further strained his and his family’s finances.
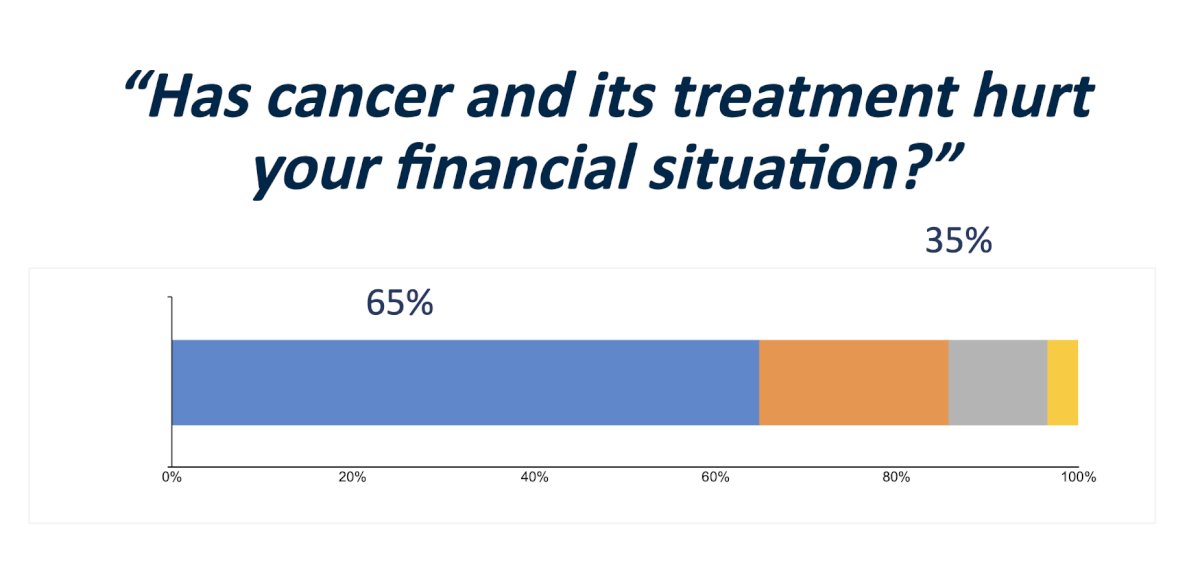
To quantify financial toxicity, the study utilized data from the Health Information National Trends – Surveillance Epidemiology and End Results (HINTS-SEER) survey. This included responses from 348 urologic cancer patients, representing an estimated 100,000 individuals, with the majority being prostate cancer sufferers. In his presentation of study results, Dr. Dhir outlined that the analysis revealed significant financial distress among these patients: 42% had depleted their assets two years post-diagnosis, and 38% faced financial insolvency after four years. Using weighted multivariate regressions, the authors identified that older age decreased the likelihood of financial toxicity, with odds ratios suggesting that individuals aged 60-69 and 70 or above were significantly less likely to report increased financial burden compared to younger age groups. In contrast, gender analysis revealed that females experienced greater financial toxicity compared to males, with an odds ratio of 3.04. However, this was not statistically significant across all intervals.
Education level and household income also played crucial roles. Patients with higher education and income levels reported lower financial toxicity, suggesting a disparity in how financial strain affects different socioeconomic groups. Specifically, those with at least a college education or household incomes over $100,000 annually showed a decreased likelihood of reporting severe financial issues. These findings not only illuminate the significant financial challenges faced by urologic cancer patients but also emphasize the need for systemic solutions to mitigate financial toxicity.
Dr. Dhir ended his talk by not only highlighting the pressing issue of financial toxicity but also calling for interventions to alleviate this burden. Some potential solutions include targeted interventions that could include policy reforms to improve insurance coverage, reduce out-of-pocket costs, and support programs that help patients manage the financial impact of cancer treatment. He emphasized that awareness regarding risk factors for early identification of at-risk patients may aid in the development of targeted strategies to help mitigate the financial impact on vulnerable populations within the urologic cancer community.
Presented by: Apoorv Dhir, MD, University of Michigan, Ann Arbor, Michigan
Written by: Ruchika Talwar, MD, Urologic Oncology Fellow, Vanderbilt University Medical Center, during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


