(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3 and May 6, 2024, was host to the advanced prostate cancer moderated poster session. Dr. Daniele Robesti presented the results of a single-center cohort of patients with a negative PSMA-PET for biochemical recurrence (BCR) after radical prostatectomy (RP) and explored the role of PSA doubling time (PSADT) in patient stratification.
Dr. Robesti started by discussing why it's still unclear whether a negative PSMA PET scan can completely rule out significant recurrent disease in patients with BCR after RP. They aimed to determine if we can safely delay salvage treatments, and if any reliable clinical factors can predict early clinical progression after a negative PSMA PET scan for BCR.
The study analyzed 136 patients with a negative PSMA-PET for BCR after RP. Notably, the investigators decided to exclude all patients with BCR treated with salvage radiation therapy (n=60). The primary outcome of this study was early clinical progression, which was defined as any new metastasis within 12 months after a negative PSMA PET.
The investigators used multivariable Cox regression to examine early clinical progression, adjusting for several variables:
- ISUP grade (≤7 vs. 8-10)
- PSA at the time of PSMA-PET
- PSADT
- pN status (pN0/x vs. pN1).
Dr. Robesti began by noting that nearly half (45%) of the cohort had an ISUP grade of ≥4, and 18% had pN1 disease. They explored different PSA and PSADT values using cubic splines analyses. In cubic spline analysis, non-linearity in predicting metastatic progression was observed at 6 months of PSADT (C-index 0.699).
In the multivariable Cox regression analysis, PSADT<6 months (HR 3.1, p=0.01) and ISUP grade ≥ 4 (HR 2.4, p=0.01) were found to be associated with an increased risk of early clinical progression. However, the PSA level at the time of PSMA-PET was not found to be significant.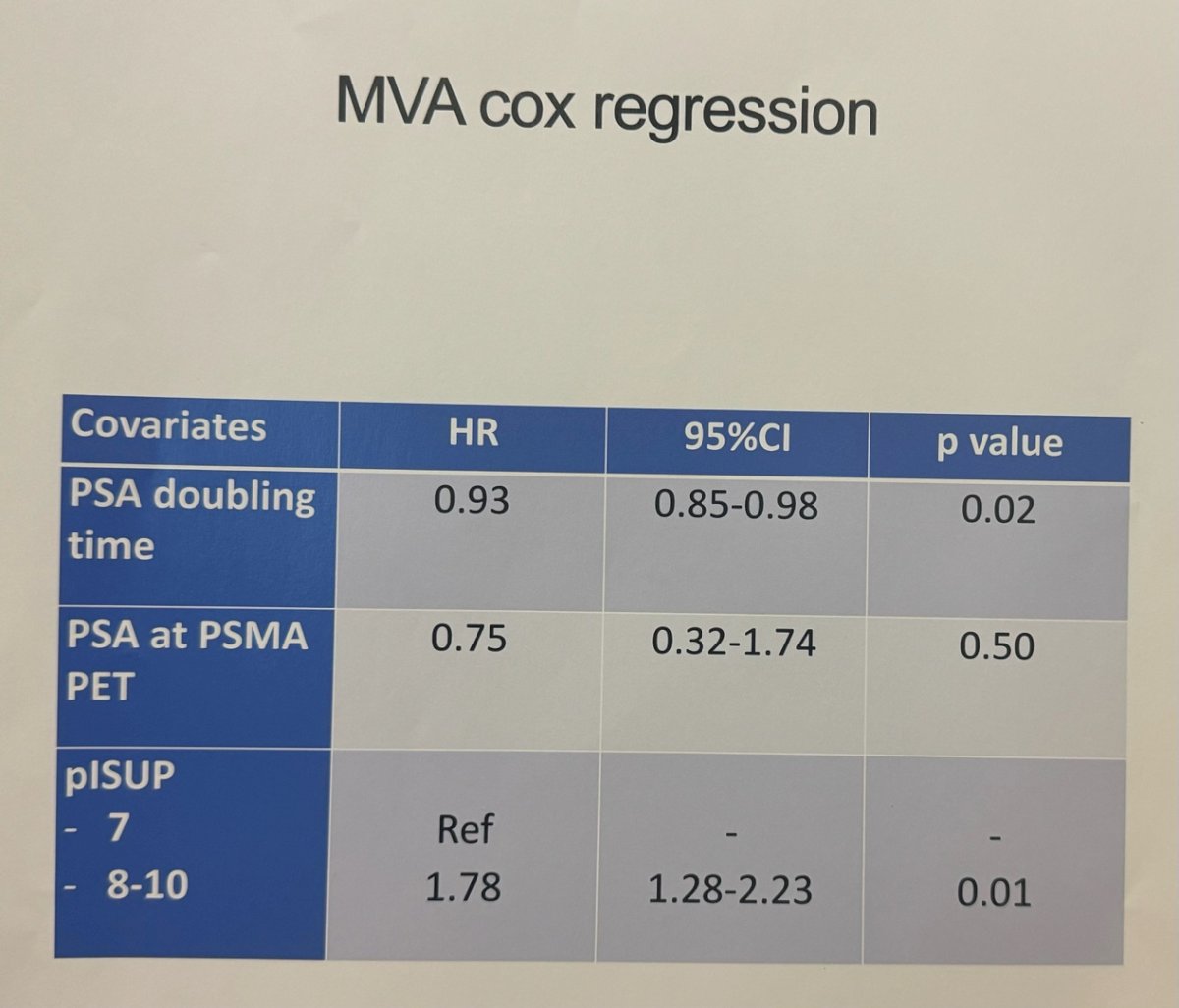
Additionally, they utilized a regression tree analysis to stratify patients into three risk group categories: low risk, intermediate risk, and high risk. They evaluated the accuracy and net benefit of the proposed three-risk-group model using the area under the curve (AUC) and decision curve analysis (DCA). The risk of clinical progression varied according to each proposed risk group: 2% for low-risk, 16% for intermediate-risk, and 33% for high-risk. 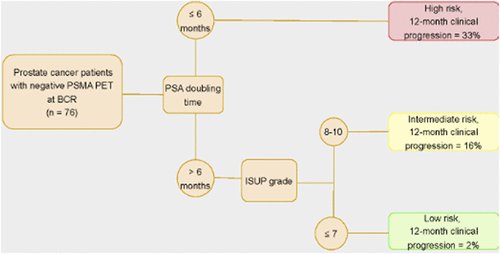
The model depicted good discrimination (AUC 0.74) and higher net benefit at DCA when their model was compared to the European Association of Urology EAU biochemical recurrence risk groups (AUC 0.68). The DCA graphic is shown below: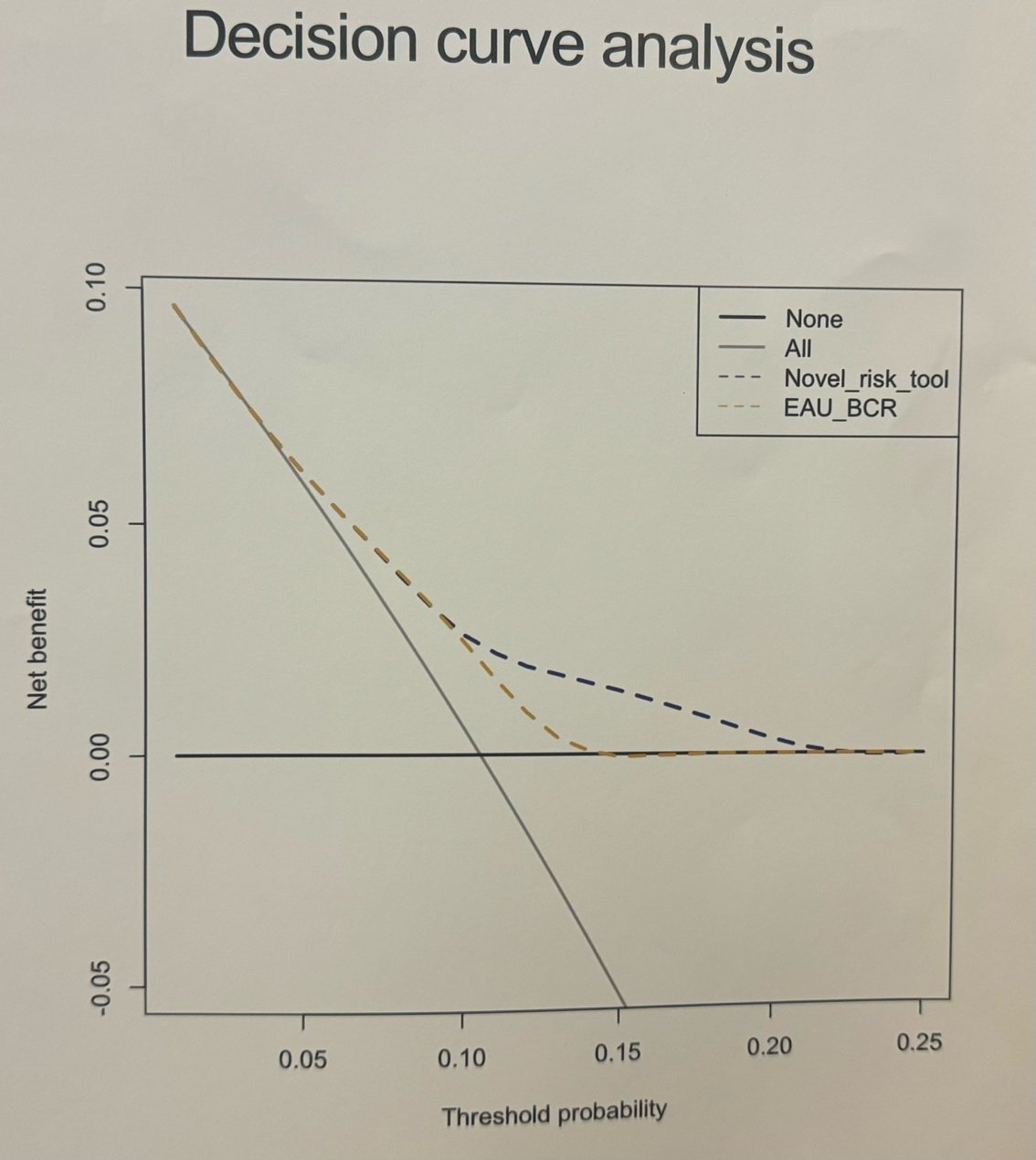
The presenter ended his presentation by concluding that PSADT and ISUP grade can optimize the identification of patients at higher risk for early metastatic progression after a negative PSMA-PET for BCR after radical prostatectomy and that patients with:
- PSADT ≤ 6 months and/or
- ISUP grade ≥ 4
Would be the ideal candidates for treatment intensification, despite negative PSMA-PET imaging.
Presented by: Daniele Robesti, MD, IRCCS San Raffaele Scientific Institute, Vita-Salute San Raffaele University, Milan, Italy.
Written by: Julian Chavarriaga, MD - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3rd and May 6th, 2024


