(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3 and May 6, 2024, was host to the advanced prostate cancer moderated poster session. Dr. Elio Mazzone presented the results of a retrospective study involving patients undergoing metastasis-directed therapy (MDT) for a positive PSMA PET spot located beyond the pelvic area in individuals experiencing biochemical recurrence (BCR) of prostate cancer following radical prostatectomy. The primary aim was to assess whether concurrent whole-pelvis salvage radiation therapy provided any additional benefit in oligo recurrent prostate cancer patients receiving MDT, potentially preventing clinical recurrence.
Dr. Mazzone began his presentation by highlighting the efficacy of metastasis-directed therapy (MDT) in reducing the risk of progression among patients with recurrent prostate cancer and positive PSMA PET scans indicating oligorecurrent disease. However, he noted that given the potential for PSMA-PET to miss micro-metastatic local recurrences, some patients might benefit from additional concomitant whole-pelvis salvage radiation therapy (WPRT) alongside MDT.
This retrospective analysis comprised 76 patients treated with MDT for confirmed oligo recurrent prostate cancer based on positive PSMA-PET findings between 2006 and 2022. MDT involved stereotactic ablative radiation therapy (SABR) targeting positive spots, including both nodal and bony lesions. The primary endpoint was clinical recurrence (CR), defined as the detection of new metastases on imaging following the initial PSMA-PET scan. Among the cohort, 39 patients received concomitant WPRT, with 58% having extra pelvic nodal spots and 52% exhibiting bony PSMA-positive lesions. The median number of PSMA spots was 1 (IQR 1-3).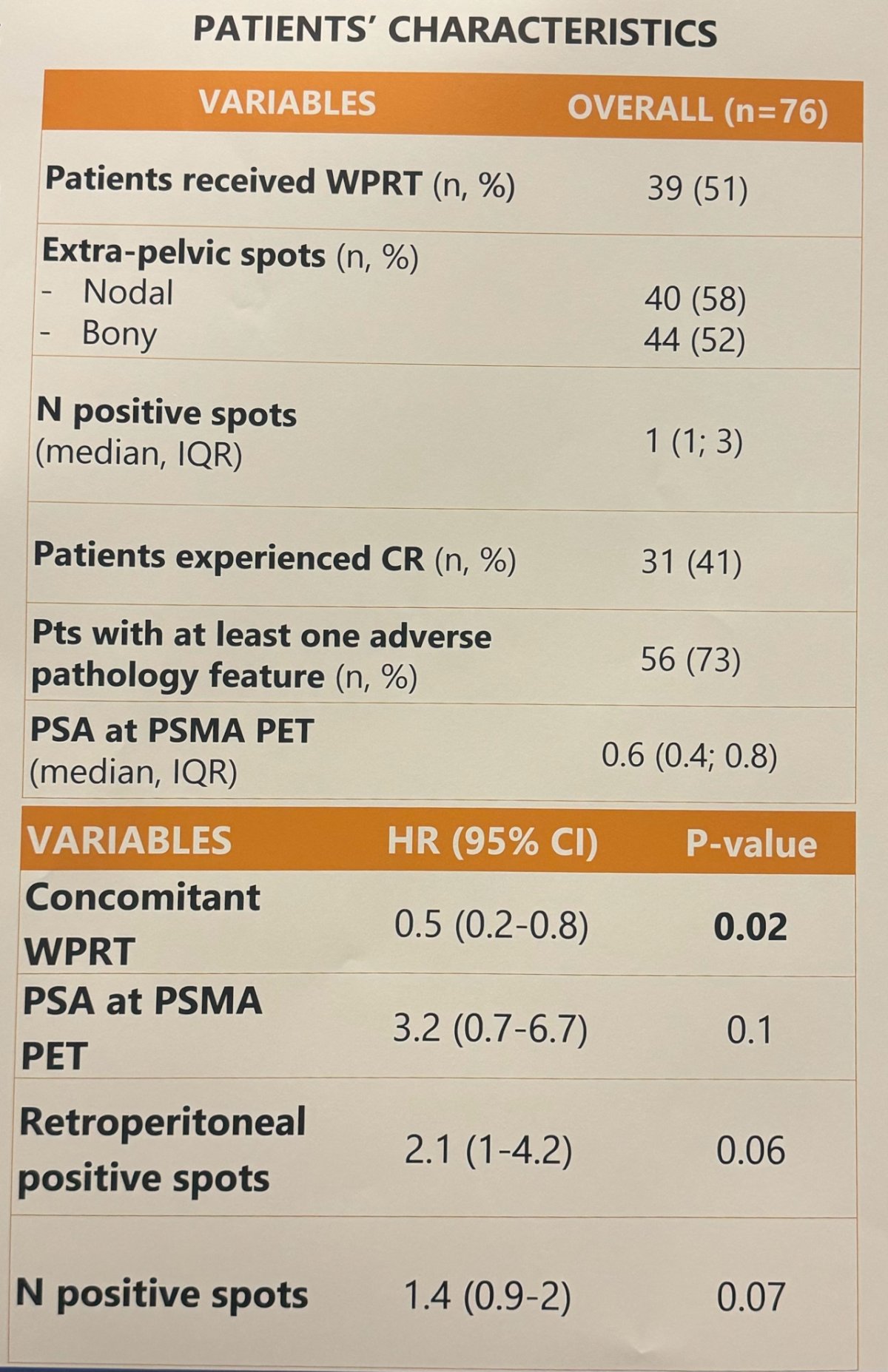
To explore the association between WPRT at the time of MDT and clinical recurrence they used multivariable Cox regression models, the variables included for analysis were:
- Number of positive spots
- Location of positive spots (retroperitoneal nodes vs bone)
- Androgen-deprivation therapy (ADT) use.
In Cox models, concomitant WPRT demonstrated a significant association with reduced risk of clinical recurrence (HR, 0.5; p=0.02). Moreover, when integrated into Cox models considering the individual risk of clinical recurrence, WPRT showed the most substantial benefits in cases where the clinical recurrence risk at 3 years exceeded 10%.
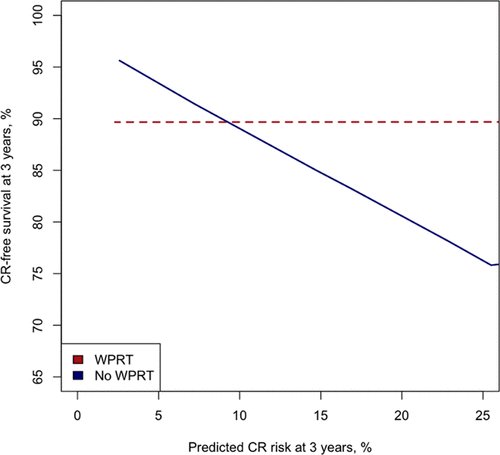
Dr. Mazzone concluded his presentation by stating that adding WPRT to MDT in patients with positive PSMA-PET oligo recurrent prostate cancer can reduce the risk of clinical recurrence, particularly in those with an estimated 3-year clinical recurrence risk exceeding 10%. However, he also emphasized that MDT alone can be a safe approach for men with oligo recurrent disease on PSMA-PET, especially those with a low risk of metastatic progression at 3 years (<10%).
Presented by: Elio Mazzone, MD, PhD, Urologic Oncologist, Vita-Salute San Raffaele University, Milan, Italy
Written by: Julian Chavarriaga, MD - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3rd and May 6th, 2024


