(UroToday.com) The 2024 American Urological Association (AUA) Annual Meeting held in San Antonio, TX was host to a prostate cancer detection and screening moderated poster session. Dr. Giuseppe Chiarelli presented the results of an analysis comparing midlife baseline PSA as a predictor of lethal prostate cancer between Black and White men.
Numerous prior reports have evaluated prostate cancer mortality based on midlife baseline PSA, defined as the first PSA test performed between 40 and 59 years of age. However, these reports have mostly included ‘homogenous’ populations, and thus there is a need to investigate this in racially/ethnically diverse populations. The objective of this study was to investigate racial differences in the predictive value of midlife baseline PSA for lethal prostate cancer, defined as death from prostate cancer or the development of metastatic disease in a diverse, contemporary, North American population.
This study included Black and White men aged 40–59 years who underwent a midlife baseline PSA between 1995 and 2019 at the Henry Ford Health system. Patients were divided into four categories based on age:
- 40 to 44
- 45 to 49
- 50 to 54
- 55 to 59
Midlife baseline PSA was operationalized as a dichotomous variable, based on PSA level above/below the median in the entire cohort and for each group. Receiver Operating Characteristic (ROC) curves and Area Under the ROC Curve (AUC) were used to compare the performance of midlife baseline PSA in predicting lethal prostate cancer based on race. Cumulative incidence curves for the rates of lethal prostate cancer were generated, stratified by race and midlife baseline PSA above/below the median for the entire cohort, as well as for each age group. Multivariable competing risks modeling was used to evaluate the relationship between midline baseline PSA and its association with race on lethal prostate cancer.
A total of 112,967 men met the inclusion criteria, of whom 82,084 (73%) were White and 30,883 (27%) were Black. White patients had their first PSA most frequently performed between 50–54 years of age (33.9%) while Black patients were between 40 and 44 (27.6%). The frequency of prostate cancer diagnosis was 7% in Black patients versus 3.9% in White patients. The frequencies of lethal prostate cancer were 1.2% and 0.6%, respectively (both p<0.0001). White men harbored Gleason score 3+3 disease more frequently (23.7% versus 16%), and less frequent cM+ (12.7% vs. 15.2%), compared to Black men (both p<0.05).
The median follow-up was 6.7 (IQR 2.9 - 14.4) years for White patients and 9.9 (4.4 - 16.4) years for Black patients. On multivariable analysis, using White patients with a PSA below the median as the reference group, the hazard ratios of lethal prostate cancer for White men with PSA >median aged 40-44, 45-49, 50-54, and 55-59 were 3.0, 3.0, 5.1, and 3.4, respectively.
Conversely, the hazard ratios of lethal prostate cancer for Black men with PSA > median aged 40-44, 45-49, 50-54, and 55-59 were 5.5, 4.2, 9.8, and 7.5, respectively (p for all <0.001).
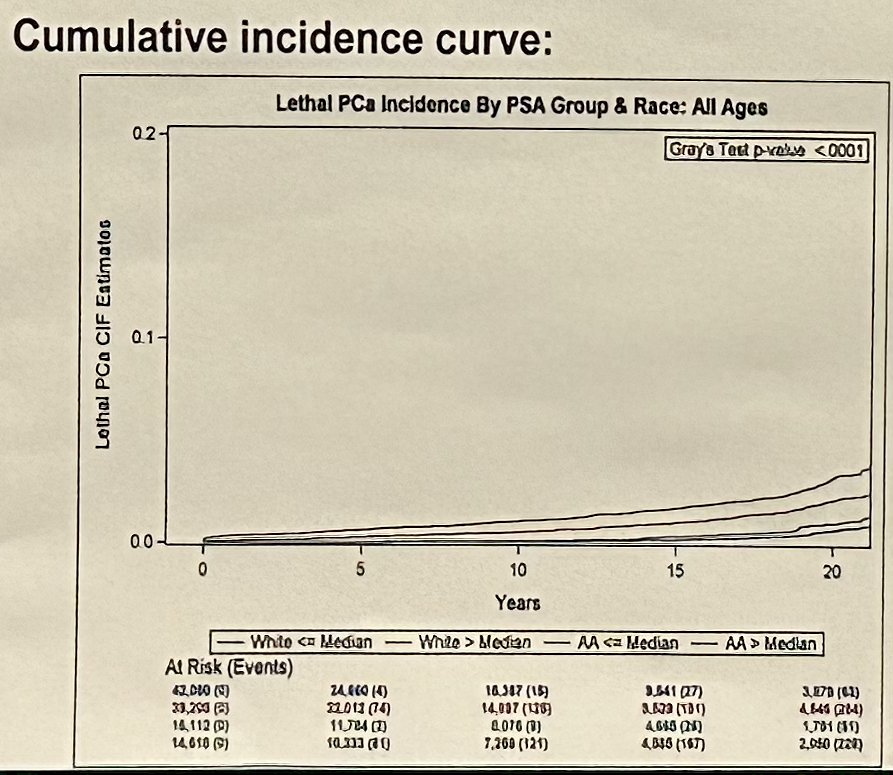
Dr. Chiarelli concluded that these findings suggest that for the same midlife baseline PSA, and within the same age category, Black men have almost double the risk of developing lethal prostate cancer compared to White men. This implies that separate and different cut-offs should be created for midlife baseline PSA, based on race, if this is to be used to guide PSA screening in clinical practice.
Presented by: Giuseppe Chiarelli, MD, Urology Resident Physician at Humanitas Research Hospital in Milan, Italy and Research Fellow at Vattikuti Urology Institute, Detroit, MI
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


