(UroToday.com) The 2024 American Urological Association (AUA) Annual Meeting held in San Antonio, TX between May 3rd and 6th, 2024 was host to a prostate cancer moderated poster session. Dr. Eric Li presented the results of an analysis evaluating genomic signatures associated with adverse pathologic features at radical prostatectomy among active surveillance-eligible men.
Dr. Li noted that grade re-classification is common among active surveillance patients. Genomic biomarkers may risk stratify active surveillance candidates and help with patient selection for treatment decision-making. The objective of this study was to identify genomic signatures associated with adverse pathologic features at radical prostatectomy among active surveillance eligible patients.
The study cohort included patients with NCCN very low-, low-, and favorable intermediate-risk prostate cancer diagnosed between February 2012 and March 2023 who underwent a radical prostatectomy and Decipher® genomic classifier testing. The primary study outcome was adverse pathologic features at radical prostatectomy, defined as the presence of Grade Group 3–5, pT3b, and/or pN1 disease. Associations between adverse pathologic features and previously defined transcriptomic signatures derived from the Decipher GRID (PAM50, PSC, PTEN, and eleven prognostic signatures) were evaluated using the Mann-Whitney U test, Fisher’s exact test, and multivariable logistic regression analyses.
The study cohort included 112 patients. The majority of patients had favorable intermediate-risk disease (73.2%). Thirty-one patients (28%) had adverse pathologic features (upgrading to Grade Group 3–5: 90%; upgrading to Grade Group 3–5 and pT3b disease: 10%). Men with adverse pathologic features had higher baseline serum PSA levels (6.4 ng/mL vs 4.9 ng/mL, p=0.02) and were less likely to have undergone an MRI fusion biopsy for diagnosis (71% vs 90%, p=0.02). 
Seven of eleven previously characterized prognostic gene-based signatures were associated with adverse pathologic features on multivariable analysis. PTEN loss and increased activated tumoral CD4 activity were also significantly associated with adverse pathologic features.
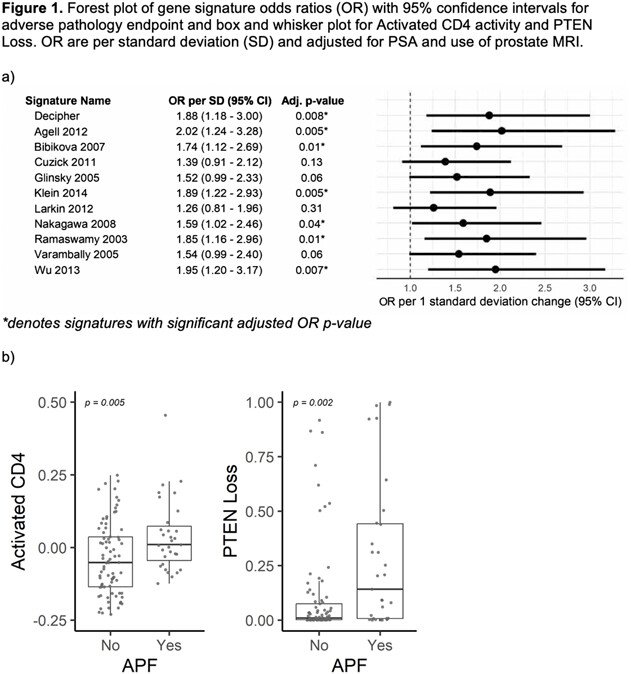
The investigators concluded that despite similar clinical features at diagnosis, active surveillance-eligible patients have significantly different outcomes and risk of adverse pathologic features due to underlying molecular heterogeneity. The Decipher genomic classifier, PTEN loss, and activated CD4 activity at diagnosis are associated with adverse pathologic features among active surveillance-eligible patients. Clinical trials within active surveillance populations should consider the utility of genomic signatures in patient selection.
Presented by: Eric Li, MD, Resident Physician, Department of Urology, Northwestern University Feinberg School of Medicine, Chicago, IL
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024


