(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a session on prostate cancer markers, and a presentation by Dr. Todd Morgan discussing the development and validation of a multimodal artificial intelligence (MMAI)-derived digital pathology-based biomarker predicting metastasis for radical prostatectomy patients with biochemical recurrence in NRG/RTOG trials.
There is a continued need to optimize the treatment of men with biochemical recurrence post-radical prostatectomy to avoid both over- and under-treatment. To date, no artificial intelligence-based models have been developed in radical prostatectomy cohorts or in the salvage radiotherapy setting. However, MMAI models have already been successfully trained from FFPE prostate biopsy samples to (i) estimate risk for distant metastasis and death from prostate cancer (prognostic biomarker),1 (ii) estimate benefit of short-term ADT with radiotherapy (predictive biomarker),2 and (iii) estimate benefit of long term ADT with radiotherapy (predictive biomarker).3 At the 2024 AUA annual meeting, Dr. Morgan and colleagues presented results developing a novel prognostic biomarker for patients with biochemical recurrence post-radical prostatectomy using multimodal deep learning on digital histopathology.
Two phase III randomized trials were identified that enrolled men post-radical prostatectomy with biochemical recurrence, NRG/RTOG 9601 and 0534. Digitized images of prostatectomy tumor samples were utilized to develop an MMAI model to predict distant metastasis utilizing image features with pathologic Grade Group, pathologic T stage, pre-salvage radiotherapy PSA, age, and surgical margin status: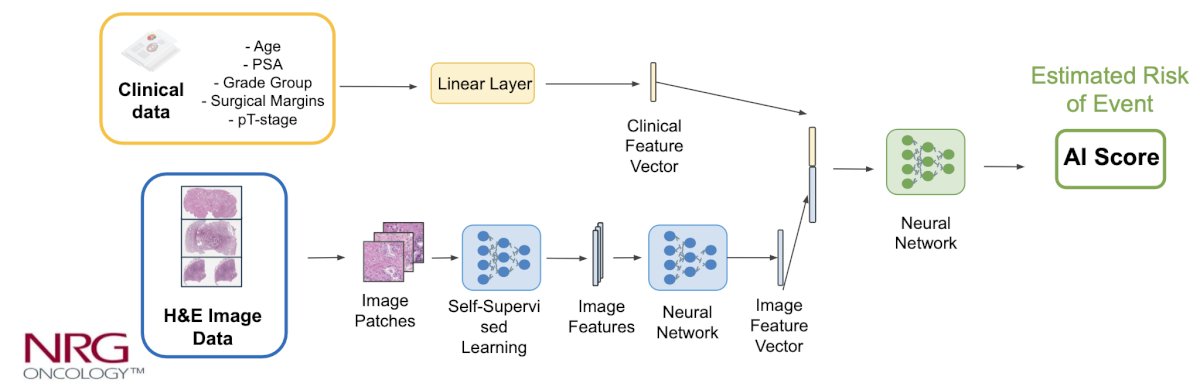
The trials were pooled and randomly split into training (70%, n = 1,322) and validation (30%, n = 533) cohorts, and the model was locked prior to any validation analyses. The model performance was evaluated using Fine and Gray’s regression for distant metastasis: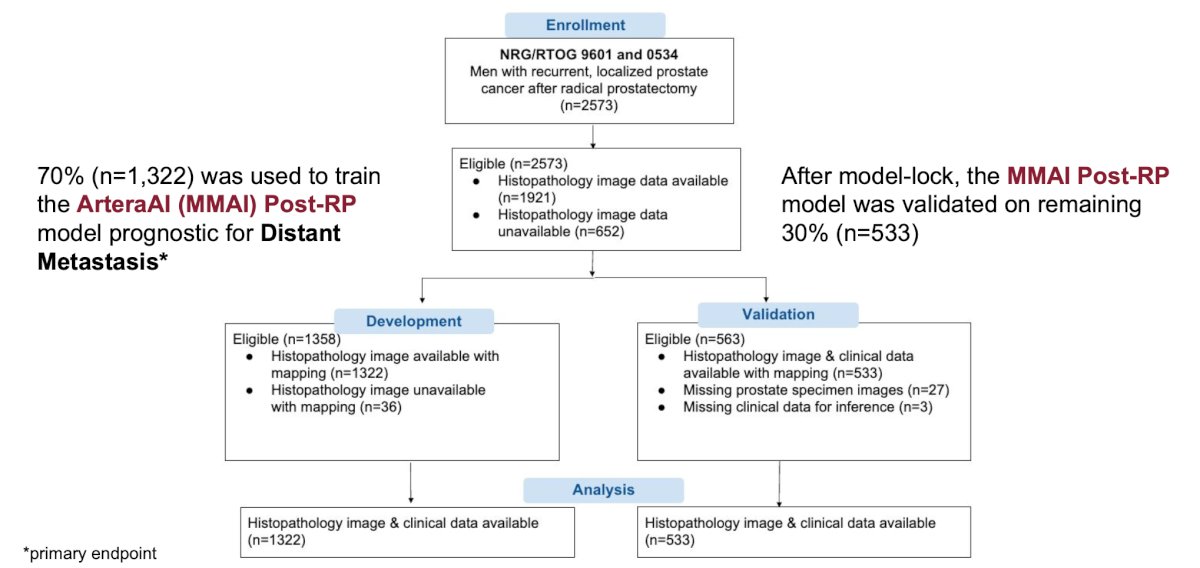
Clinical and histopathological data were available for 1,855 of the 2,556 eligible patients (72.6%). The training cohort included 1,322 men (median follow-up of 9.3 years, IQR [7.3, 11.5]), and the validation cohort included 533 men (median follow-up of 9.2 years, IQR [7.1, 11.3]), with a median pre-salvage radiotherapy PSA of 0.4 ng/mL in the overall cohort. Of note, 54% were pT3 and 17% were pathologic Gleason Score 8-10: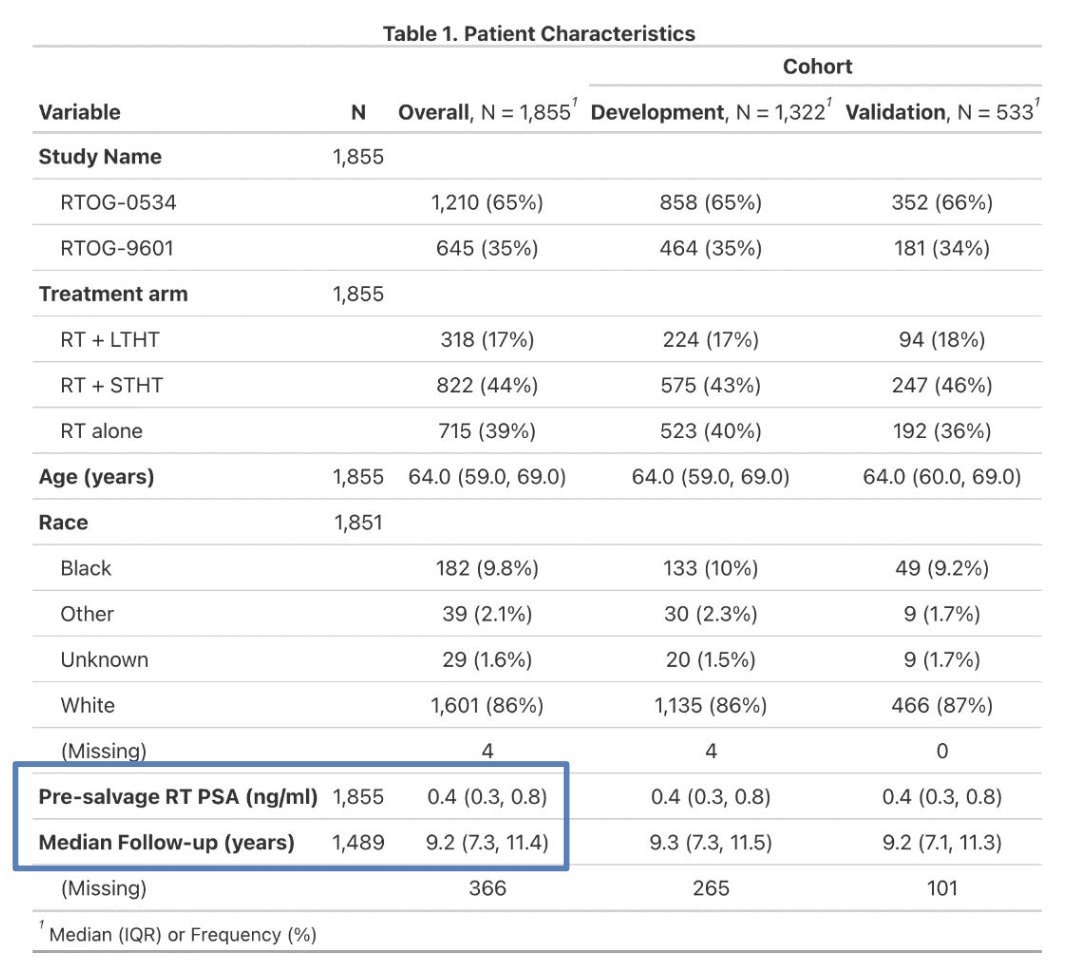
An optimized MMAI model score cut-off was selected to group 212 (40%) patients as higher risk and 321 (60%) patients as lower risk. The estimated 10-year cumulative incidence of distant metastasis rates were 27.0% (95% CI 19.9%-34.1%) in the higher risk group and 8.7% (95% CI 5.3%-12.2%) in the lower risk group (p < 0.001):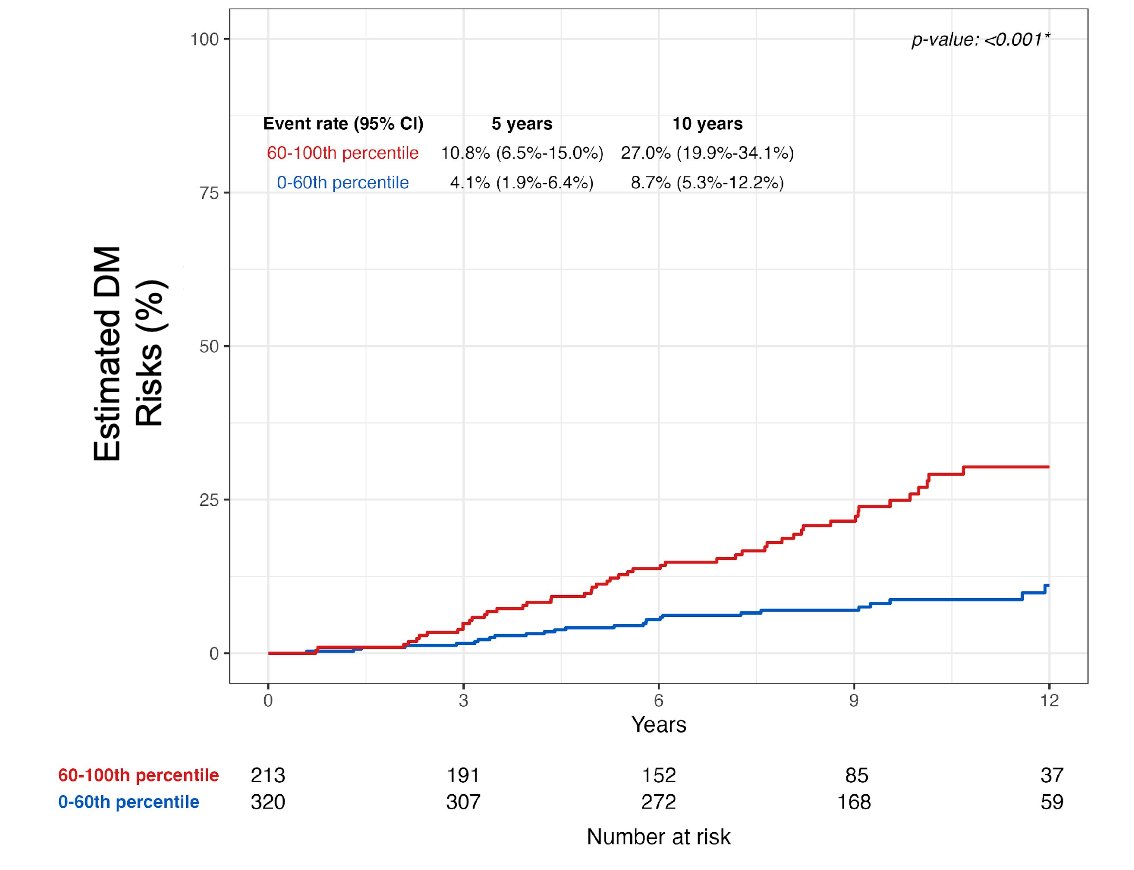
The post-radical prostatectomy model was strongly associated with long-term outcomes, including distant metastasis, death with distant metastasis, prostate cancer-specific mortality, biochemical failure, freedom from progression, metastasis-free survival, and overall survival: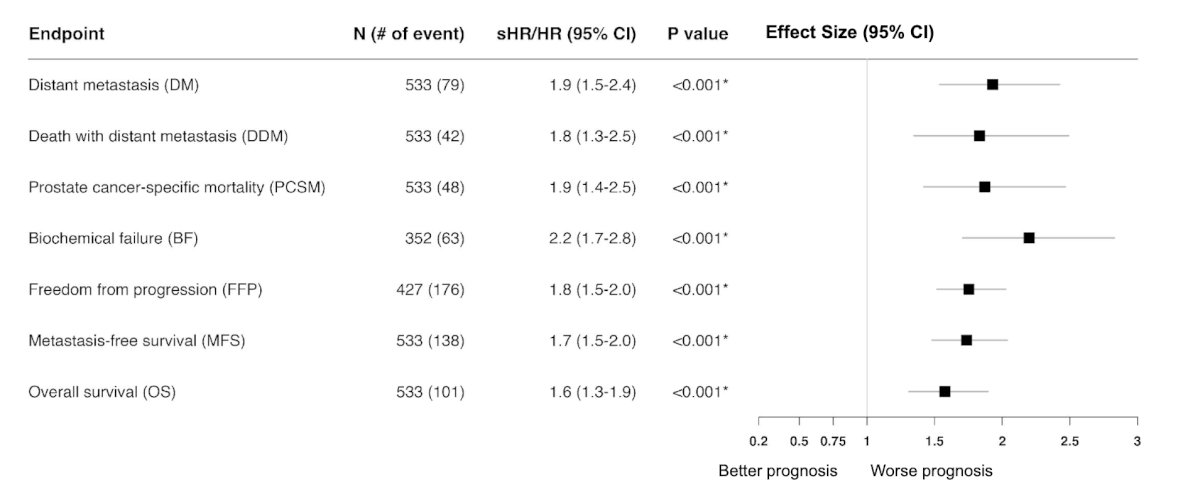
The subgroup analyses for distant metastasis is as highlighted as follows: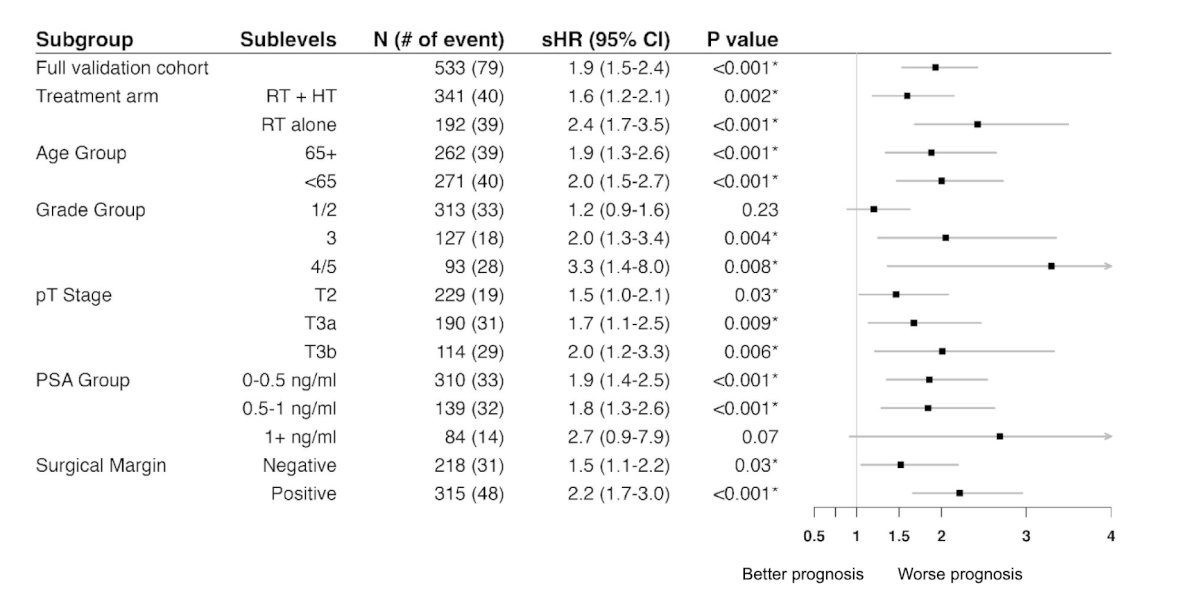
Among MMAI higher-risk patients (n = 213), patients treated with radiotherapy alone had a 10-year cumulative risk of metastases of 41% (95% CI 29%-54%) compared to 18% (95% CI 10%-26%) for those treated with radiotherapy + hormone therapy (HR 2.16, 95% CI 1.25 – 3.72, p = 0.006):
Among MMAI lower-risk patients (n = 320), patients treated with radiotherapy alone had a 10-year cumulative risk of metastases of 10% (95% CI 4%-16%) compared to 8% (95% CI 4%-12%) for those treated with radiotherapy + hormone therapy (HR 1.21, 95% CI 0.57 – 2.58, p = 0.62):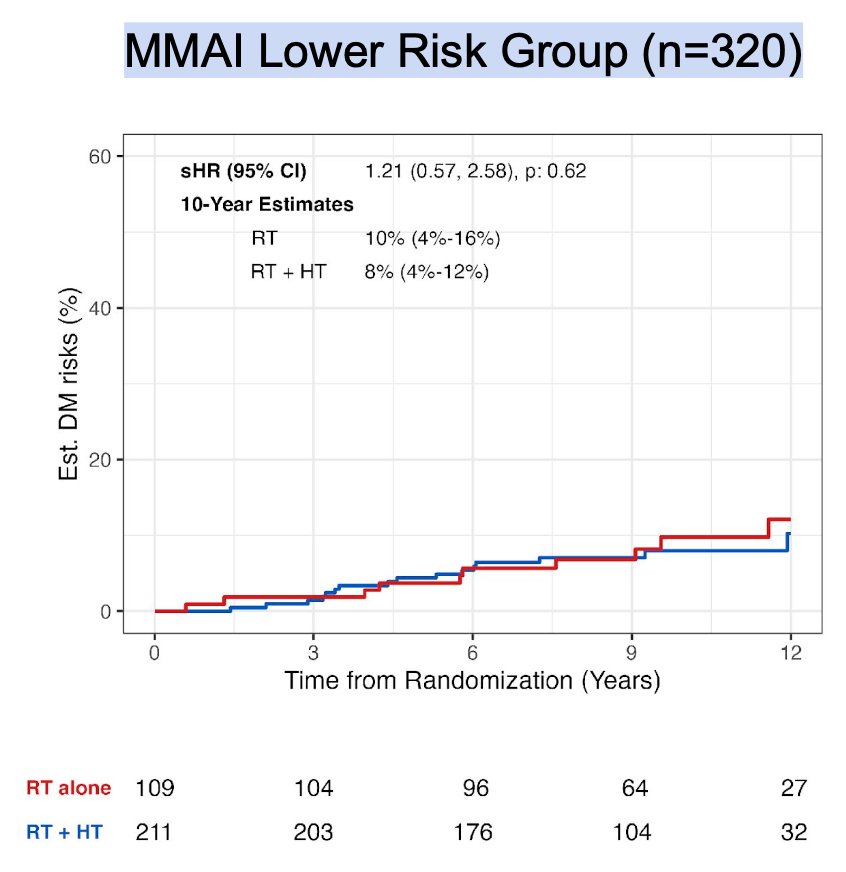
Finally, Dr. Morgan highlighted that the post-radical prostatectomy model is largely driven by tissue image features (34.6%):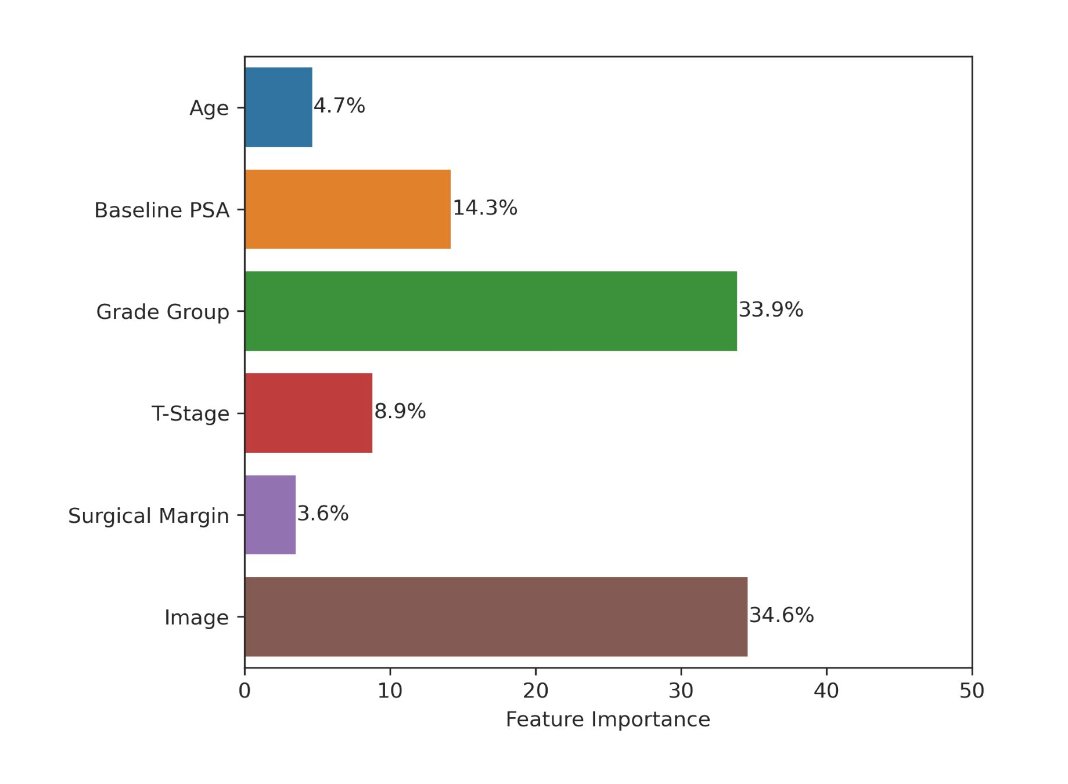
Dr. Morgan concluded his presentation discussing the development and validation of an MMAI-derived digital pathology-based biomarker predicting metastasis for radical prostatectomy patients with biochemical recurrence in NRG/RTOG trials with the following take-home messages:
- The MMAI post-radical prostatectomy is the first that has been trained and validated using completed phase III trials of men post-prostatectomy and is prognostic for all tested endpoints
- This biomarker is able to identify differential absolute benefit for the addition of hormone therapy to salvage radiotherapy and may aid in personalization of treatment for these patients
Presented by: Todd Morgan, MD, Urologist, University of Michigan, Ann Arbor, MI
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 - Mon, May 6, 2024.
Related content: Predicting Response to Hormone Therapy in Prostate Cancer With a Post-Prostatectomy MMAI Model - Todd Morgan
References:
- Esteva A, Feng J, van der Wal D, et al. Prostate cancer therapy personalization via multi-modal deep learning on randomized phase III clinical trials. NPJ Digit Med. 2022 Jun 8;5(1):71.
- Spratt DE, Tang S, Sun Y, et al. Artificial Intelligence Predictive Model for Hormone Therapy Use in Prostate Cancer. NEJM Evid 2023;2(8).
- Armstrong A, et al. Development and validation of an AI-derived digital pathology-based biomarker to predict benefit of LT-ADT with RT in men with localized high-risk prostate cancer across multiple phase III NRG/RTOG trials. ASCO 2023.


