(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a session on prostate cancer markers, and a presentation by Dr. Nimrod Barashi discussing the variation in prostate cancer genomic subtypes across prostate MRI PI-RADS scores and race. Multi-parametric magnetic resonance imaging of the prostate (mpMRI) and genomic classifiers are being increasingly used for risk stratification of localized prostate cancer. mpMRI has many benefits, including standardized reporting with PIRADS, a good NPV for Gleason Grade Group >= 2 prostate cancer, allows for targeted prostate biopsies, and provides clinical staging. The Decipher genomic classifier is tissue based (from prostate biopsy or prostatectomy), assessing the expression of 22 RNA biomarkers, including AR signaling, cell proliferation, and immune modulation. Additionally, the Decipher genomic classifier has been validated externally in multiple studies. Current clinical uses of the Decipher genomic classifier include:
- Active surveillance
- The addition of short term ADT to radiotherapy in intermediate risk prostate cancer
- Long versus short term ADT + radiotherapy in high risk prostate cancer
- The addition of ADT to early radiotherapy after biochemical recurrence
Using the largest cohort of racially diverse men with mpMRI and genomic classifier data from initial biopsy, Dr. Barashi and colleagues sought to evaluate the correlations between imaging and tumor genomic findings. Additionally, they also explored differences between African Americans and non-African Americans.
The investigators retrospectively identified patients at their institution who underwent an mpMRI + biopsy + Decipher genomic classifier testing (Veracyte, San Diego, CA) between December 2016 to March 2023. Genomic signatures were then developed from GRID, followed by a correlation between Decipher score and PIRADS. Stratification was also performed by race and then re-assessed. Fisher’s exact test was used to evaluate the association between PIRADS 1-2 vs 3-5 and four tumor subtyping classifiers (PAM50, PCS, ERG, and pTEN) obtained from the Decipher GRID research database in the full cohort and stratified our cohort by race.
There was a total of 760 patients included, with 612 (81%) non-African Americans and 132 (17%) African Americans. The most common PIRADS was PIRADS 4 (37%) and PIRADS 5 (34%):
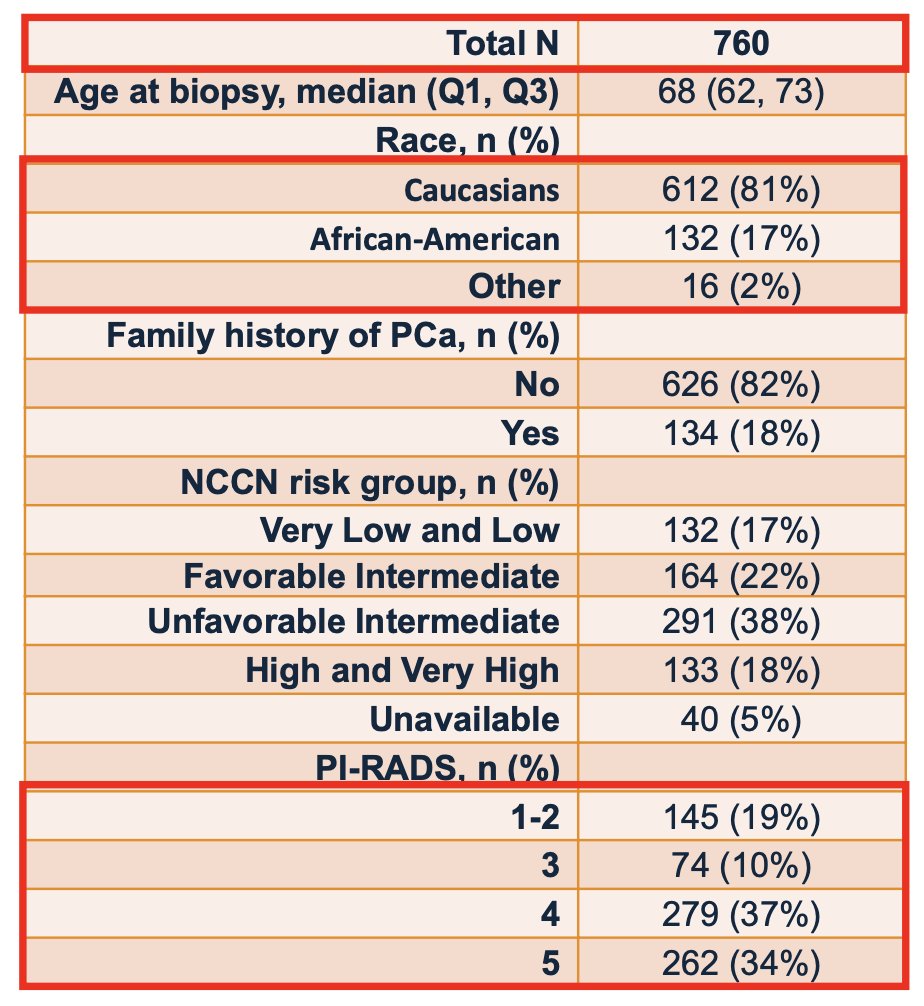
The median Decipher score was 0.43 (IQR 0.27, 0.64), with 53% being in the low Decipher risk group, 18% in the intermediate risk group, and 29% in the high risk group:
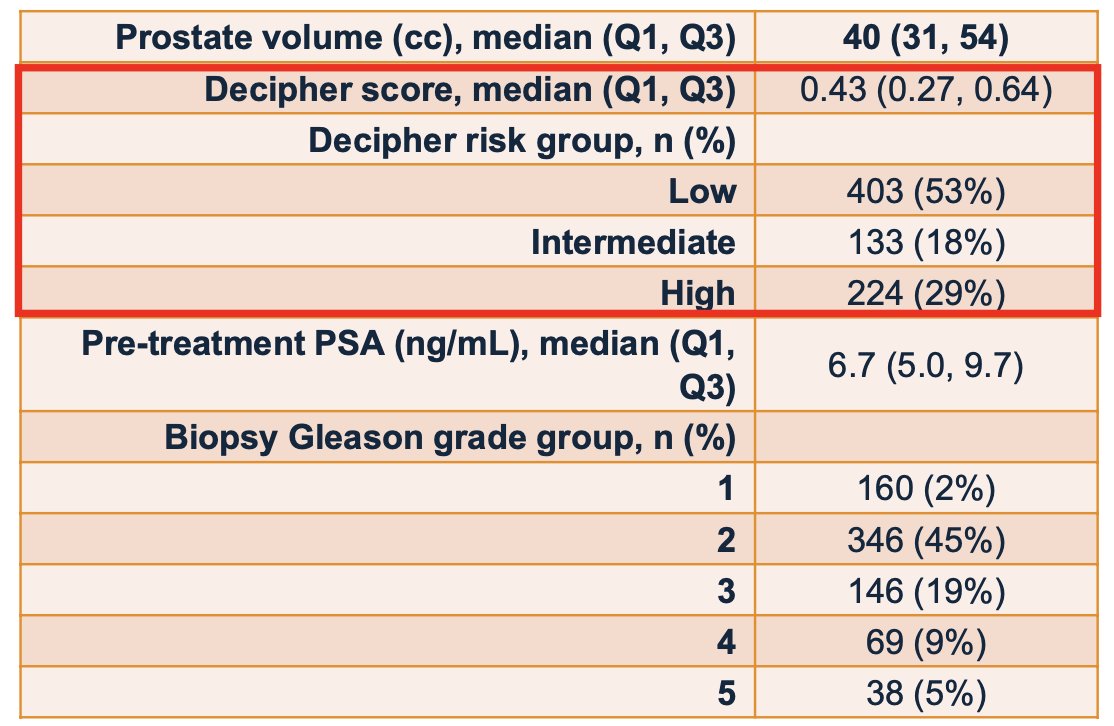
The Decipher genomic classifier generally correlated well with the PIRADS scoring system, among non-African Americans and African Americans only, albeit somewhat weaker for African Americans:
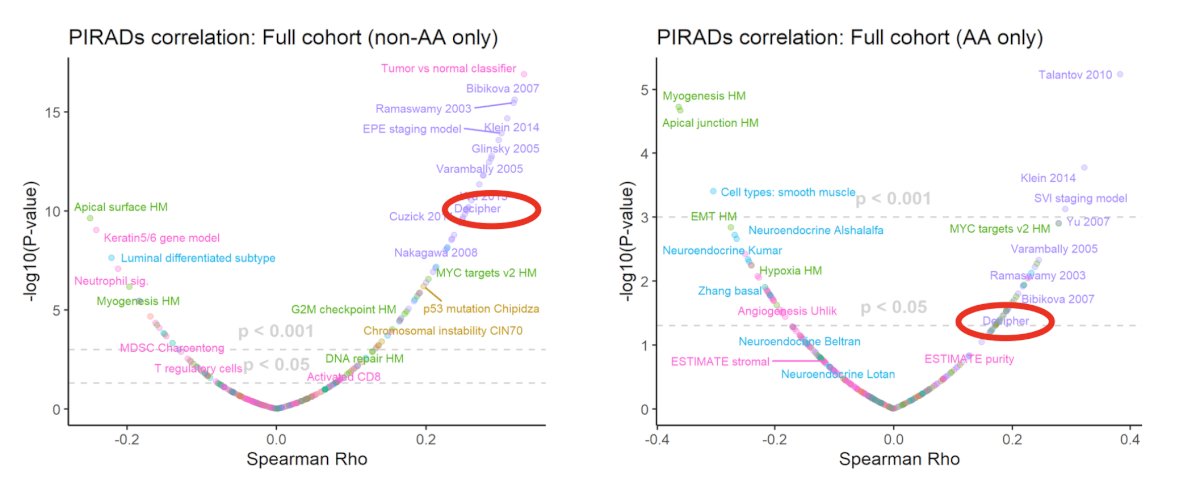
In aggregate, PIRADS 3-5 lesions harbored enrichment for more aggressive prostate cancer subtypes like luminal proliferating (31% vs 17%, p = 0.004) and luminal B (45% vs 31%, p = 0.001), compared to PIRADS 1-2:
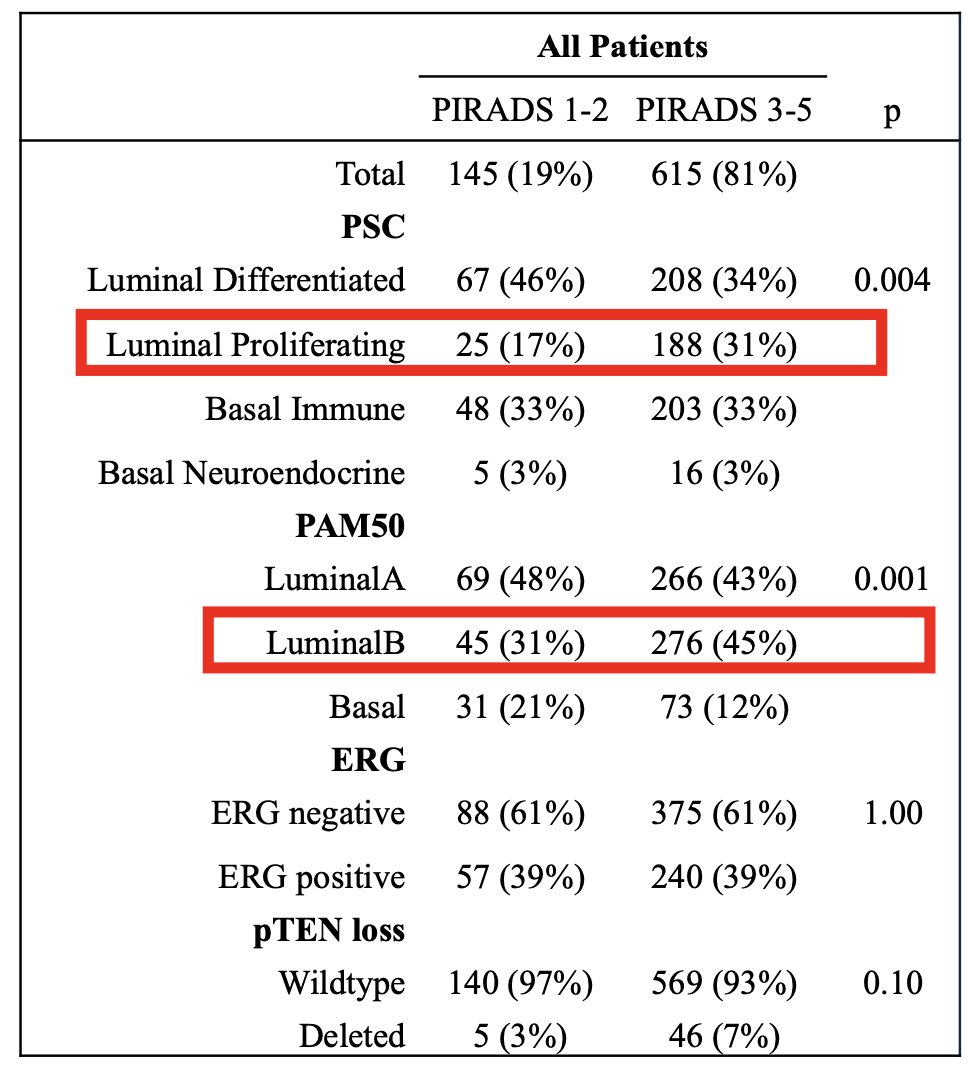
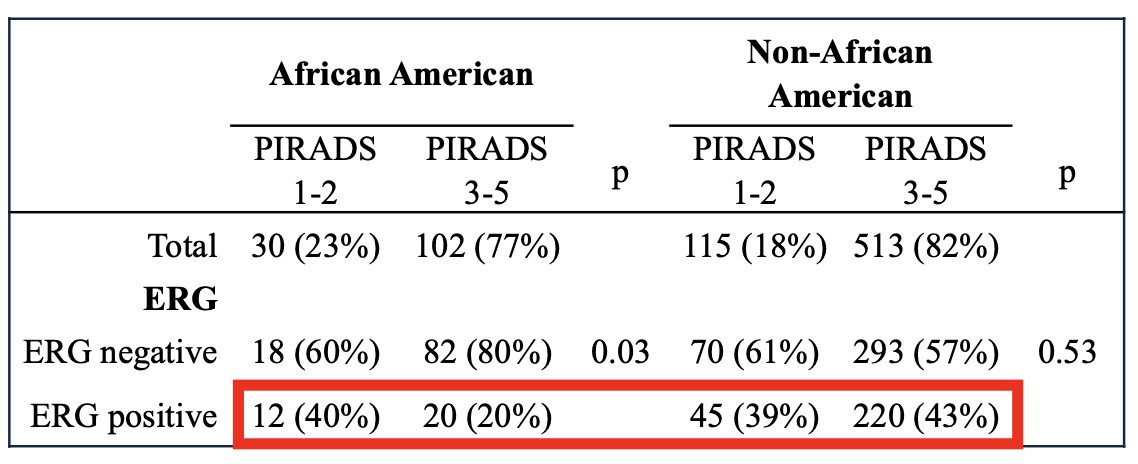
The same correlation is maintained in the non-African Americans, with PTEN deletions more common in patients with PIRADS 3-5 (8% vs 3%, p = 0.04). Variation in ERG subtype across PIRADS was most pronounced in African Americans subset, where prevalence of ERG was similar to non-African Americans in PIRADS 1-2 (40% and 39% ERG positive, respectively) but markedly lower in the PIRADS 3-5 tumors (20% vs. 43% ERG positive, respectively):
Dr. Barashi notes that there are several ongoing questions:
- MRI “positivity” traditionally is attributed to histology and tumor volume, but what is the role of genomics?
- What are the genomic differences between African Americans and non-African Americans with prostate cancer?
- What is the role of artificial intelligence and radiomics incorporating genomic data?
Dr. Barashi concluded his presentation by discussing the variation in prostate cancer genomic subtypes across prostate MRI PI-RADS scores and race with the following take-home messages:
- This was a large, diverse cohort of men with prostate cancer, and both MRI and Decipher data
- The Decipher score correlated well overall with MRI findings, however, this correlation is weaker for African Americans
- Men with positive MRIs usually harbored more aggressive subtypes of prostate cancer overall, but this was not the case for African Americans
Presented by: Nimrod S. Barashi, MD, Washington University, St. Louis, MO
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


