(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3 and May 6, 2024, was host to the Focal Therapy Society (FTS) Session at AUA. Dr. Kae Jack Tay discussed the epidemiology applied to focal therapy in Prostate Cancer: (PCa).
Dr. Tay opened his talk by defining focal therapy. He stated that the aim of focal therapy is to eliminate the cancer focus while preserving uninvolved tissue and maintaining the patient's quality of life by avoiding damage to adjacent structures (neurovascular bundles, urinary sphincter). There are different modalities of focal therapy, including targeted ablation, which targets a region of interest; quadrant ablation, targeting a specific quadrant of the prostate; anterior zone ablation, which treats the anterior zone of the prostate including the fibromuscular stroma; hemiablation, treating half of the gland; and hockey stick, used when treating bilateral disease but preserving uninvolved tissue of the less-involved prostatic lobe.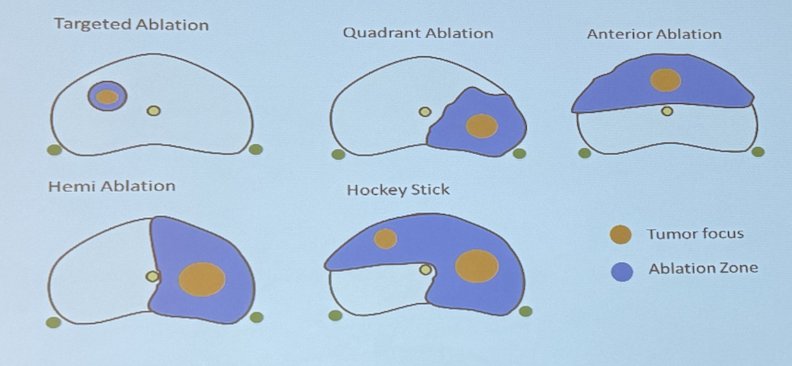
He proceeded to discuss how with new diagnostic and screening tools such as magnetic resonance imaging, we have been able to more accurately detect regions of interest in the prostate and specifically target them during prostatic biopsy. So the question he posed to the audience is, if we are improving our methods of diagnosis and finding more clinically significant prostate cancer, how does this better and more accurate diagnosis impact the epidemiology of prostate cancer, and how does the epidemiology of prostate cancer ultimately impact focal therapy?
Dr. Tay affirmed that prostate cancer is the most common cancer diagnosed in men worldwide, and its incidence ranges from 24 per 100,000 ASR in Western Asia to 82.8 per 100,000 in Northern Europe. He highlighted how mortality is not only correlated with the incidence of prostate cancer but also with the geographical area where the diagnosis is made.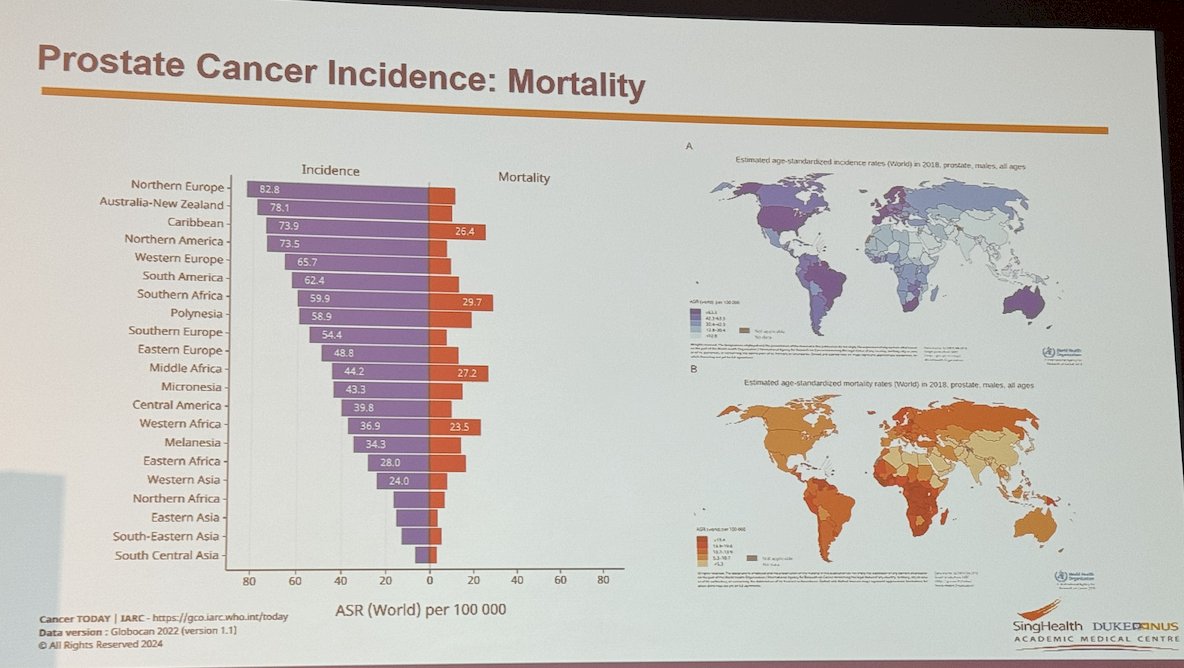
As our understanding of prostate cancer has advanced, we've recognized that many cases do not require treatment, and these patients often pass away with the disease rather than from it. In a systematic review encompassing 29 autopsy studies, the incidence of PCa increased with each decade of life, with an odds ratio of being diagnosed with PCa ranging from 1.7 to 2.0 per decade.
Dr. Tay quoted a study by Johansson et al., who assessed the frequency of death from prostate cancer by analyzing 223 patients over a 32-year follow-up period. Among these patients, 41% experienced localized progression, 18% developed metastasis, and 90% died; however, only 17% died of prostate cancer. Furthermore, he discussed a study analyzing 50,066 men with PCa in the United Kingdom (UK), where approximately 20% of individuals died of prostate cancer. However, among patients with localized prostate cancer (Stage I), the mortality rate was much lower at 11.2%.
Age and Gleason scores correlate significantly with the mortality rate of PCa. With increasing age, there is an increase in mortality. However, with an increasing Gleason score, PCa mortality increases dramatically, according to the study by Albertsen et al. cited by Dr. Tay, please refer to the figure below.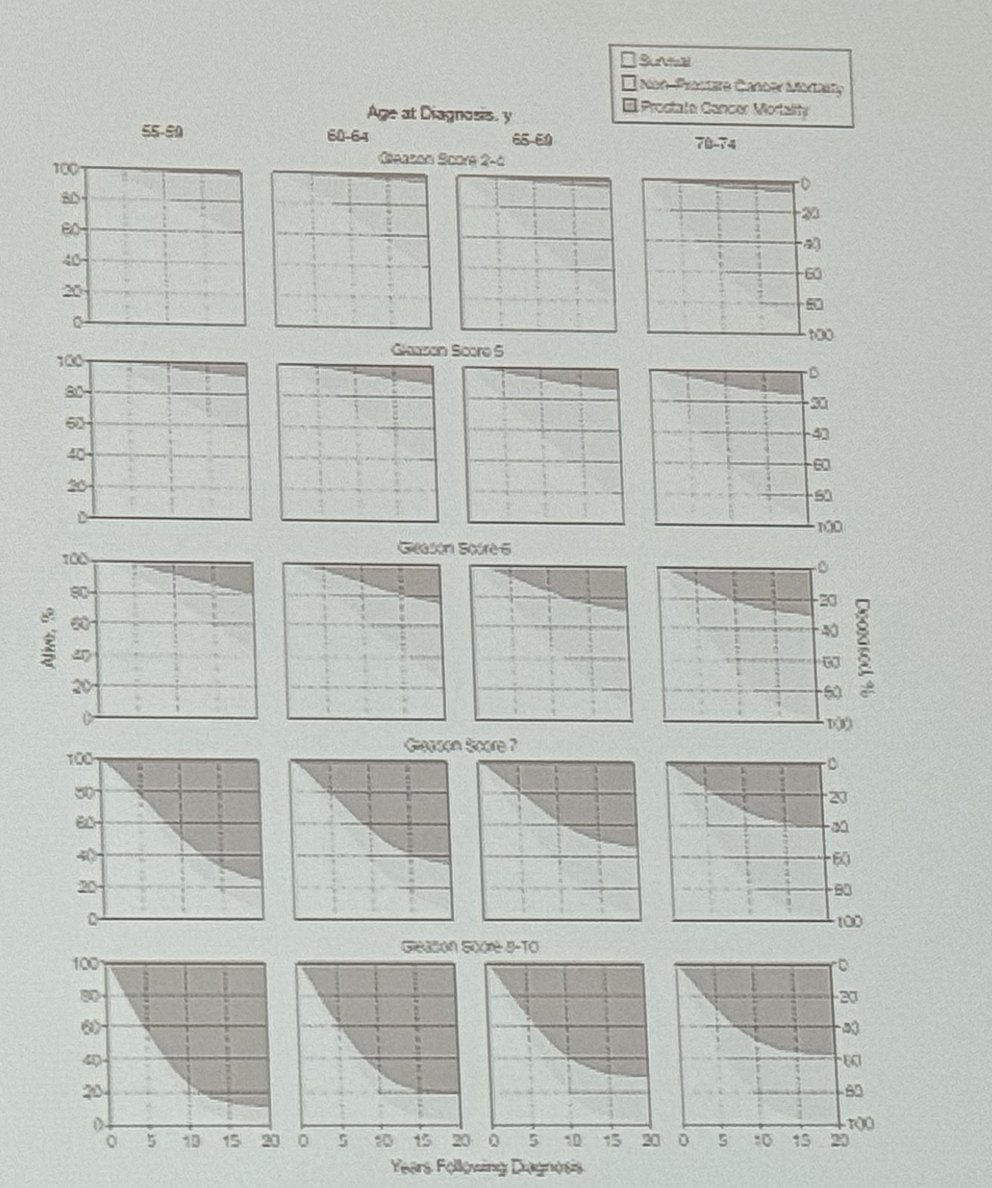
Dr. Tay discussed watchful waiting in men with PCa and quoted a study involving 204 men in Singapore diagnosed with PCa, with a median follow-up of 12 years. During this time, 19 men died from prostate cancer, while 84 died from other causes. Predictors of overall mortality included Charlson comorbidity index and age, while predictors of PCa-specific mortality were grade and risk group.
Furthermore, he discussed the SPCG-4 study, involving 695 Scandinavian men under 75 years with a life expectancy of over 10 years and localized disease (≤ T2, PSA < 50, negative bone scan), the overall mortality was 166 out of 347 (47.8%) in patients treated with radical prostatectomy compared to 201 out of 348 (57.8%) in the watchful waiting group. This study demonstrated that men treated required less use of androgen deprivation (a difference of 25.0 percentage points; 95% CI, 17.7 to 32.3) and there was a significant reduction in the risk of death from prostate cancer in men younger than 65 years of age (relative risk, 0.45) and in those with intermediate-risk PCa (relative risk, 0.38).4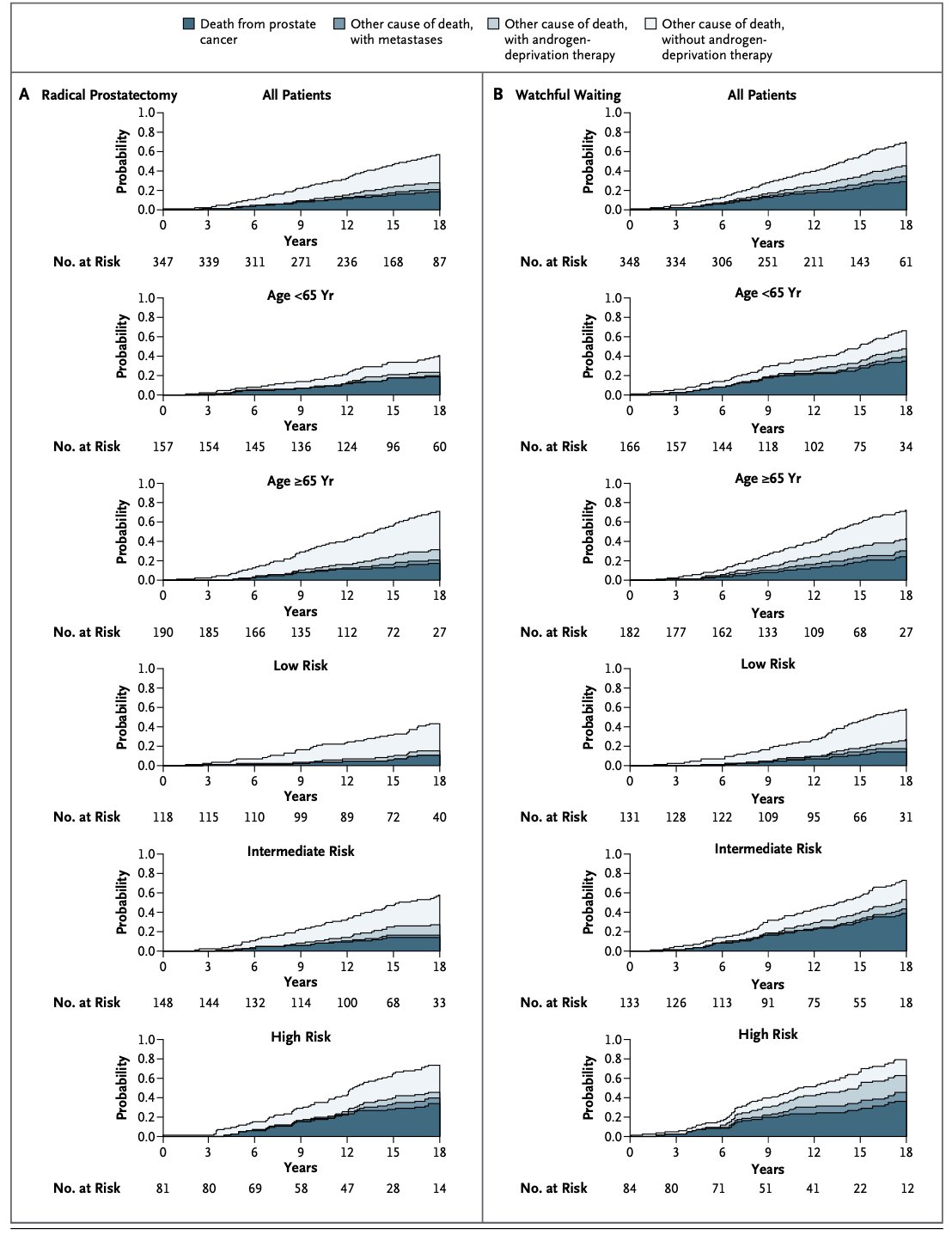
Moving on from watchful waiting, Dr. Tay discussed contemporary active surveillance series, including cohorts from Toronto, Johns Hopkins, UCSF, and The Royal Marsden. He noted that most of these series included patients with low-risk prostate cancer, except for the Toronto and UCSF cohorts, which were more flexible and included patients with intermediate-risk PCa. Overall, the cancer-specific survival at 15 years was 94% in Toronto and 99% in Johns Hopkins. The metastasis rate was low in both sites at 15 years, 1.3% and 0.25%, respectively, and it was 0.1% at 5 years in the UCSF cohort and 0.4% at 5 years in the Royal Marsden cohort. He highlighted that despite this, the treatment-free rate decreased over time, being 55% at 15 years in Toronto and 43% at 15 years in Johns Hopkins. Please refer to the table below.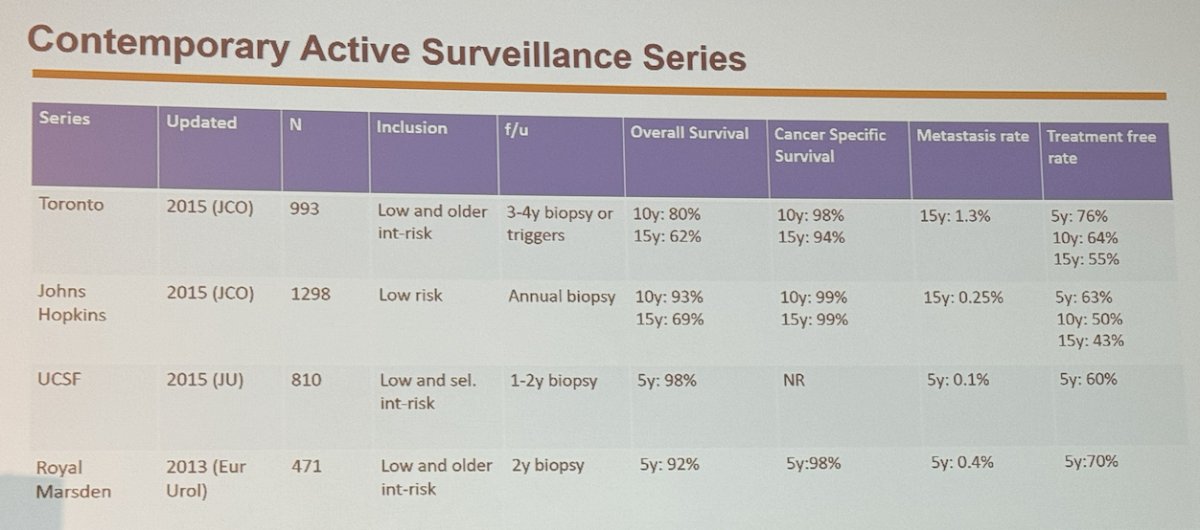
Dr. Tay moved on to say that the next question we should ask ourselves is if intermediate-risk PCa fares worse than low-risk on active surveillance. He presented data from extended follow-up of patients with intermediate-risk PCa managed with active surveillance from Toronto (Sunnybrook). They found an increased risk of metastasis (HR 3.14, p=0.001), overall mortality (HR 2.13, p<0.001), and requiring treatments during follow-up (HR 1.42, p=0.01) when compared with low-risk patients on active surveillance. Additionally, in patients with ISUP grade 3 disease, the metastasis-free survival at 15 years was 63%, and in ISUP grade 2, it was 83.6%.5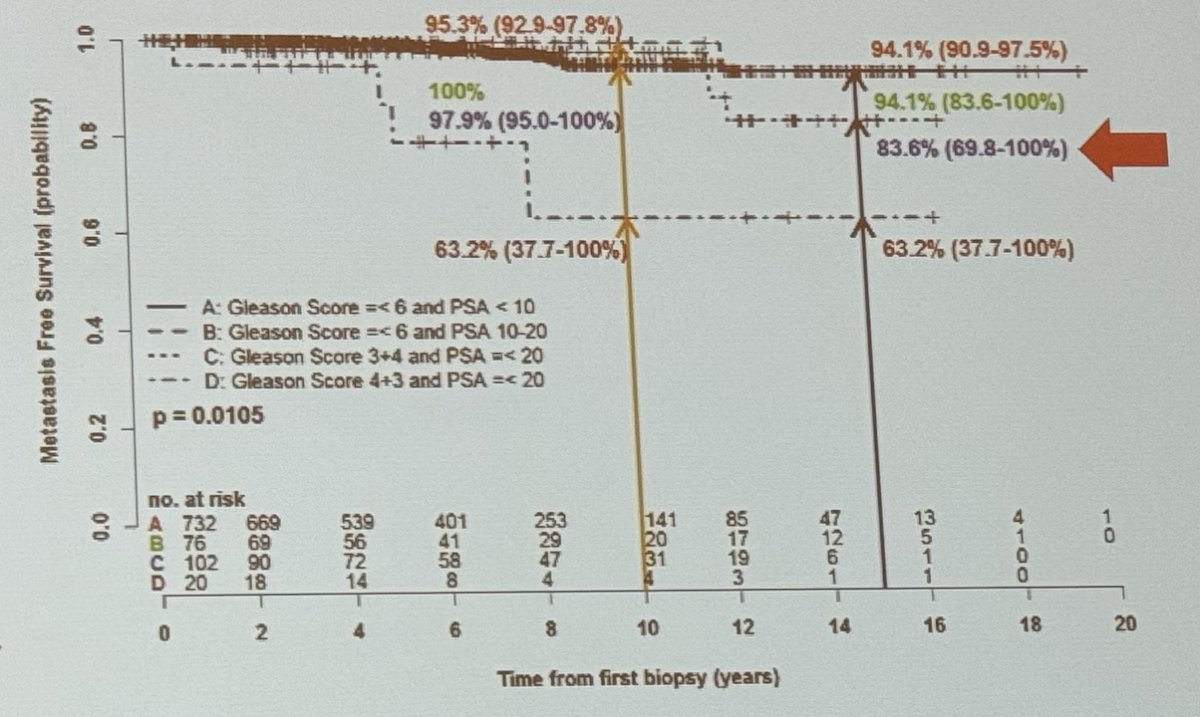
Dr. Tay then discussed The PROstate Testing for Cancer and Treatment (ProtecT) trial, this study evaluated 82,429 men who underwent PSA testing between 1999 and 2009. Of these, 82,429 screened men, 2,965 were diagnosed with prostate cancer, of whom 1,643 were randomly assigned to:
- Active monitoring: 545
- Radical prostatectomy: 553
- Radical radiotherapy: 545
This study showed that Survival from clinically localized prostate cancer remains very high over a median of 15 years (96%) irrespective if they receive active treatment or not. However, there is a higher incidence of metastases in the active monitoring group, this did not correspond to worse cancer survival outcomes.6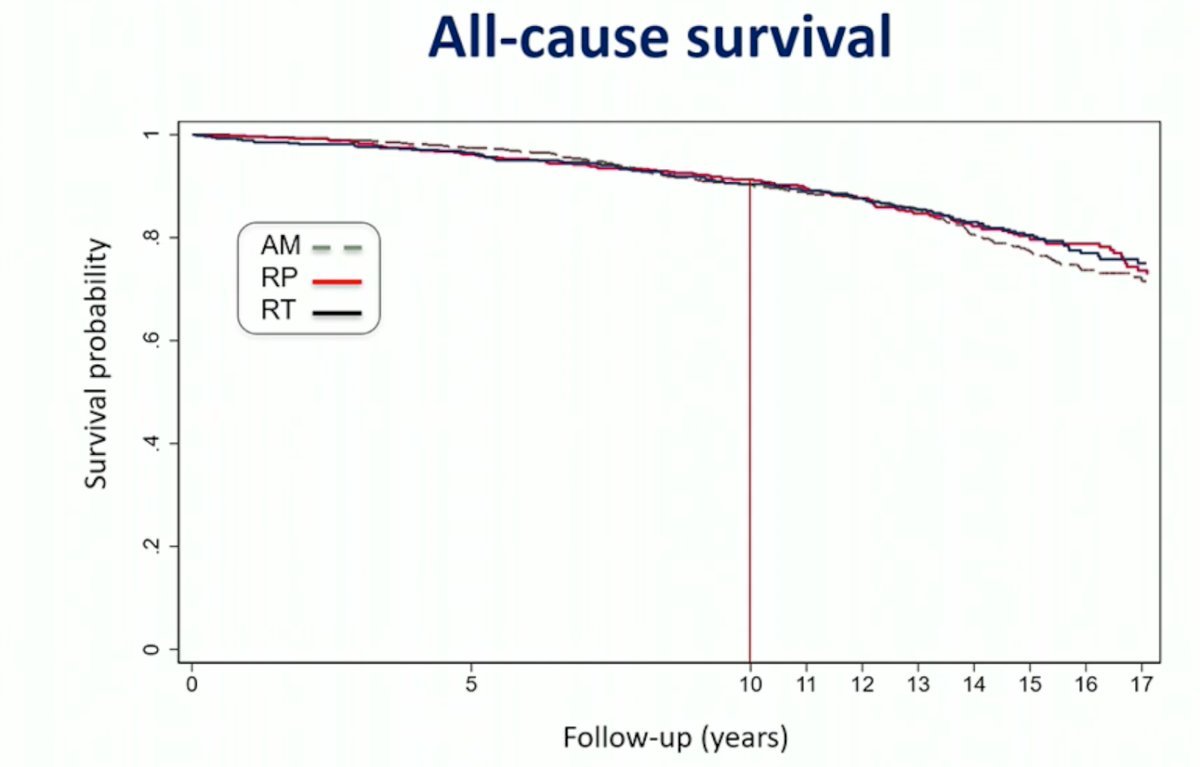
Dr. Tay then went on to discuss how we rationalize all this data and choose curative treatment options for these patients. He mentioned that, for now, the space of focal therapy is in patients with intermediate to low stage (≤ 2 foci of cancer).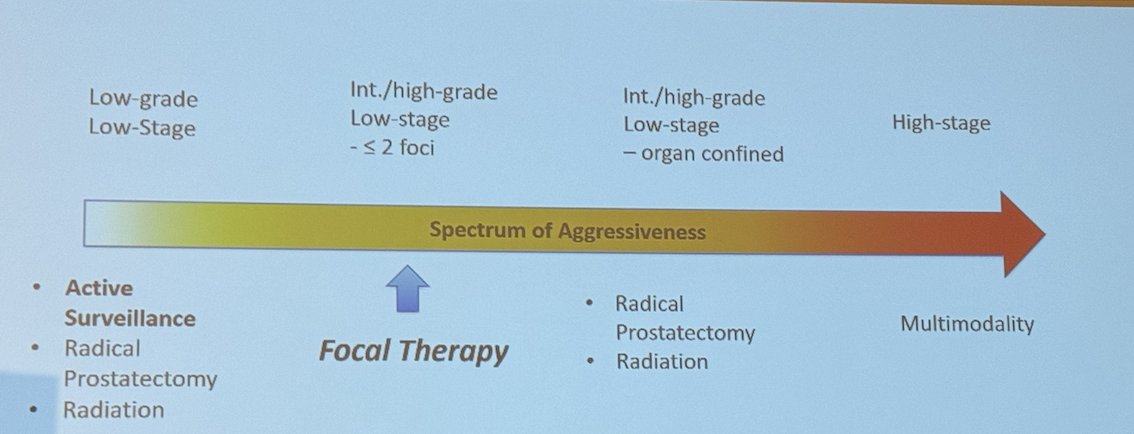
He mentioned there has to be a consensus regarding patient selection for focal therapy and that the goal of treatment has evolved over time. Initially, the goal of focal therapy was the eradication of clinically significant PCa; more recently, the goal should be to completely ablate cancer and to delay or avoid radical therapy.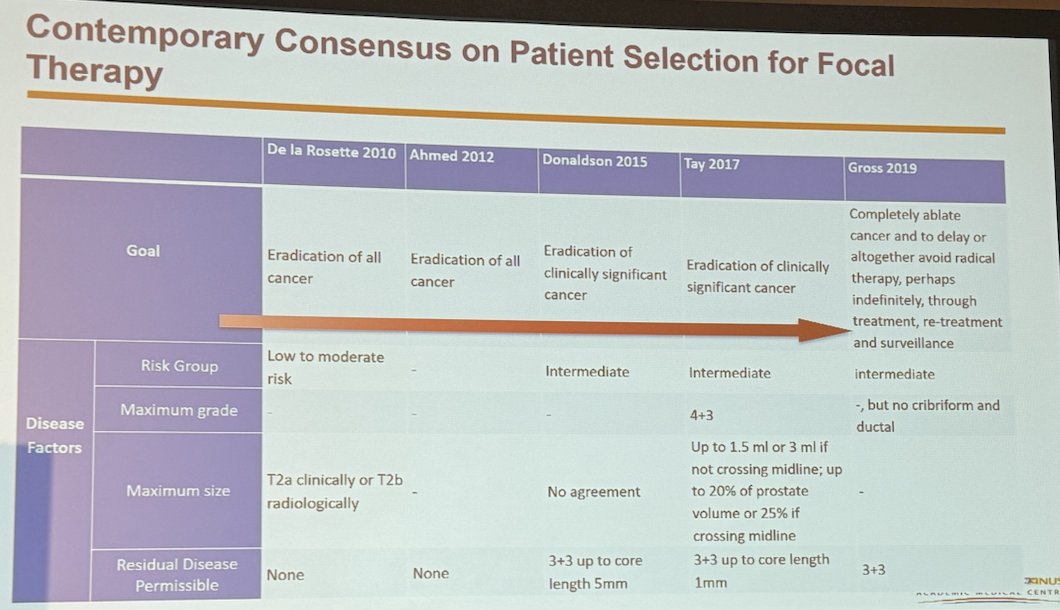
Dr. Tay mentioned that not all men are suitable for focal therapy, with approximately less than 1 out of 7 men being suitable for a focal approach, and 1 out of 6 men being suitable for hemiablation. However, with increasing life expectancies, there will be a growing number of patients who could eventually become candidates for focal therapy.
He then highlighted the importance of using transcriptomic profiles and genomic profiling to improve patient selection for focal therapy. This area is currently unexplored and requires more focus.
Dr. Tay concluded his talk by leaving the following messages:
- With an aging population, there will be an increase in the detection of prostate cancer.
- Longer life expectancy will extend treatment indications to older age groups.
- With PSMA PET/CT, MRI, and PSA, we will detect smaller tumors at an earlier stage that could potentially be treated with focal therapy.
- Estimations of genomic risk may help us better select and treat patients with focal therapy.
Presented by: Kae Jack Tay MD, Director of Urologic Oncology, Singapore General Hospital, Singapore
Written by: Julian Chavarriaga, MD - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3rd and May 6th, 2024
Related content: Epidemiology Applied to Focal Therapy in Prostate Cancer: Where do we Stand? - Kae Jack Tay
References:
- Johansson JE, Andrén O, Andersson SO, Dickman PW, Holmberg L, Magnuson A, Adami HO. Natural history of early, localized prostate cancer. JAMA. 2004 Jun 9;291(22):2713-9.
- Chowdhury S, Robinson D, Cahill D, Rodriguez-Vida A, Holmberg L, Møller H. Causes of death in men with prostate cancer: an analysis of 50,000 men from the Thames Cancer Registry. BJU Int. 2013 Jul;112(2):182-9.
- Albertsen PC, Hanley JA, Fine J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA. 2005 May 4;293(17):2095-101.
- Bill-Axelson A, Holmberg L, Ruutu M, Garmo H, Stark JR, Busch C, Nordling S, Häggman M, Andersson SO, Bratell S, Spångberg A, Palmgren J, Steineck G, Adami HO, Johansson JE; SPCG-4 Investigators. Radical prostatectomy versus watchful
- Musunuru HB, Yamamoto T, Klotz L, Ghanem G, Mamedov A, Sethukavalan P, Jethava V, Jain S, Zhang L, Vesprini D, Loblaw A. Active Surveillance for Intermediate Risk Prostate Cancer: Survival Outcomes in the Sunnybrook Experience. J Urol. 2016 Dec;196(6):1651-1658.
- Hamdy et al. Fifteen-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Prostate Cancer. New England Journal of Medicine 2023.


