(UroToday.com) The Saturday morning plenary sessions discussed men’s health screening. Dr. Mitchell Humphreys representing Mayo Clinic Arizona, Dr. Nicole Miller representing Vanderbilt University, Dr. Ricardo Gonzalez representing Houston Methodist Hospital, Dr. Christopher Tenggardjaja representing Kaiser Permanente, and Dr. Matthew Rutman representing New York – Presbyterian Allen Hospital engaged in a fascinating crossfire session regarding outlet procedures for detrusor underactivity, often referred to as TURP.
Dr. Humphreys began this crossfire session with an introduction to the topic and a quick review of the current AUA guidelines regarding surgical management of detrusor underactivity, specifically referencing outlet procedures. After this brief review, he presented a case by which the debate would be framed. In this discussion, there was a 60-year-old male with a long history of prostatitis, having 2-3 episodes per year. He presented with complaints of being unable to void, requiring intermittent catheterization (CIC) four times per day. He is currently managed with finasteride and tamsulosin and had a prior PVP procedure 5 years ago. Transrectal ultrasound measured a prostatic volume of 64.3 cm3. Results of his urodynamics studies were as follows:
- Volume: 330 mL
- PDet: 17 cmH2O
- Voided: 0 mL
- Normal compliance
- No detrusor overactivity or leakage



With this case in mind, the question was posed: to TURP or not to TURP?
Dr. Miller began the debate from the perspective of pro-surgery. Dr. Miller began her discussion by defining detrusor underactivity and highlighting the ultimate goals of treatment for detrusor underactivity, in which she highlighted reducing the need for catheterization and giving these men a chance to void volitionally. She defined detrusor underactivity via the bladder contractility index, in which a value less than 100 indicated detrusor underactivity. She highlighted the importance of this reduction in CIC not only for social convenience but also to reduce the notable side effects of CIC, among which include UTI, urosepsis, urethral stricture, bladder stones, catheter encrustation, penile erosion, quality of life and cost.
Dr. Miller continued her discussion by presenting data showing how men who have outlet surgery for detrusor underactivity achieve improved quality of life and improved spontaneous voiding in over half of the patients who get surgery. Given these generally positive results, she proceeded to question the importance of urodynamics with regard to its ability to predict voiding after surgery for patients with detrusor underactivity, to which she cited a study by Thomas et al in which no UDS finding predicted who would void or improve QOL after surgery. Dr. Miller further substantiated her argument by showing data from meta-analyses and systematic reviews, both of which showed that QOL significantly improved after surgery, regardless of the surgery performed. In sum, Dr. Miller concluded her wonderful discussion by positing that this patient in the case presentation would benefit from a TURP procedure; as such, she recommended an operation.
To open the opposing argument against TURP, Dr. Tenggardjaja took the podium. He began by re-summarizing the case presentation and brought forth the argument that there may be alternative diagnoses other than detrusor underactivity. Assuming that this patient had detrusor underactivity, he then broke his argument down into three sections: patient expectations, patient risks, and patient benefits.
Dr. Tenggardjaja began addressing patient expectations by presenting data in which 10.9% of patients reported being unaware that they would have difficulty with ejaculation after HoLEP. Furthermore, he showed how patients were significantly dissatisfied with their procedure at the 5-year mark compared with their initial expectations of their treatment outcomes.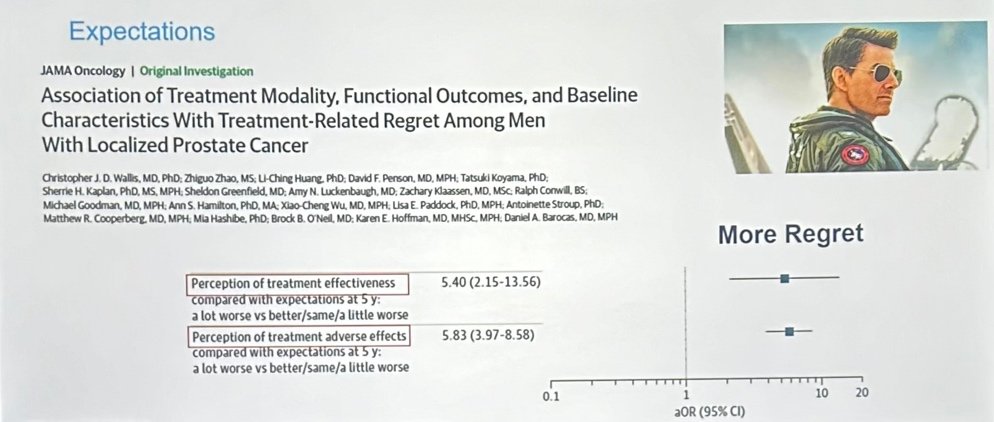
His discussion continued onto the patient risks associated with the procedure. He presented the many risks associated with TURP, among which include TUR syndrome, UTI, hematuria/clot retention, transfusion, ureteral/bladder injury, incontinence, transient retention, capsular perforation, urethral stricture/bladder neck contracture, anesthesia complications, and deep vein thrombosis. With this context in mind, he showed data in which 17 studies, 8 of which were specific to TURP, showed no difference in surgical outcomes after their procedure when comparing low vs. normal detrusor activity.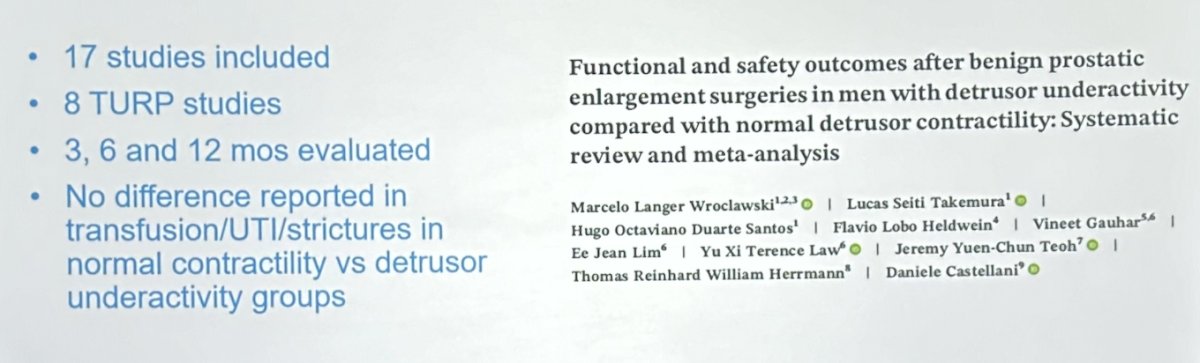
With the perspective that surgical benefit might be minimal at best, he further described the sexual dysfunction risks the patient would assume, primarily erectile and ejaculatory dysfunction, happening at 10 and 70%, respectively. With these risks, he proposes that the risks of surgery in this patient’s case would outweigh its benefits.
Dr. Tenggardjaja then moved to present data from the UPSTREAM trial, an RCT study designed as a non-inferiority trial for men comparing the urodynamics pathway to routine care, with the primary outcome being IPSS. In this trial, they showed that lower BCI, specifically less than 123, and BOOI, also less than 47.6, were both poorer predictors of surgical success.
Given this patient’s history of failed prior procedures, low BCI, and multiple risks, Dr. Tenggardjaja concluded that this patient would not benefit from surgery and that we shouldn’t make things worse for him by operating again.
Following this presentation, Dr. Gonzalez took the podium to offer a rebuttal from the perspective of pro-operation. He began by re-emphasizing the goals of treatment, which include resumption of spontaneous voiding, decreasing postvoid residual, preventing upper tract deterioration, improving quality of life, and reducing the risk of complications.
Dr. Gonzalez offered his rebuttal to Dr. Tenggardjaja by countering that choosing against operating has risks and side effects of its own, including infections, renal failure, bleeding, stones, chronic catheter use, and the idea that waiting until operations were necessary would potentially leave the patient frailer and more unable to tolerate the procedure.
Dr. Gonzalez continued his discussion by highlighting how the patient’s UDS studies were pointless, as the results it would not change the management. He proposed that regardless of the patient’s UDS results, that surgery could still be offered, and that postponement of his surgery would only increase the patient’s frailty.
On the topic of frailty, Dr. Gonzalez pointed out that the frailty index (5i-FI) was all independent predictor of 30-day post-surgical complications. As this patient was already 60 years old and only getting older, he recommended an operation, rather than “kicking the can down the road” to a point at which the patient might not be able to tolerate the procedure. By operating now, the patient’s retention would likely resolve and can be done via Anatomical endoscopic enucleation of the prostate (AEEP) with low complication rates, while postponing surgery risks waiting until the patient is older and unable to perform CIC, developing complications of chronic retention, and worsening frailty.
Following Dr. Gonzalez's rebuttal to the argument for observation, Dr. Rutman took the podium to counter the arguments made about the operation. Dr. Rutman began by rehashing the case presentation, taking time to highlight that the patient is unable to void between CIC, appears obstructed on cystoscopy, but has UDS findings not supporting obstruction.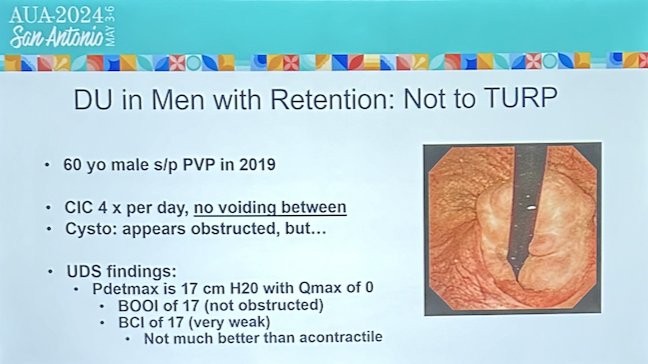
Dr. Rutman proceeded to discuss the differences between a detrusor underactivity and a contractile detrusor. He proceeded to present multiple studies, all of which supported the idea that in patients with atonic detrusors, operative vs. observational management did not have a significant difference in outcomes. Furthermore, a patient that can void between CIC is suggestive of detrusor underactivity, in which our patient does not fit the description. Rather, Dr. Rutman proposed that our patient’s history and findings are more suggestive of a contractile detrusor, in which surgical outcomes are poor. As such, he suggested that this patient would still need to catheterize regardless of treatment, therefore not benefitting from surgery and better be left alone.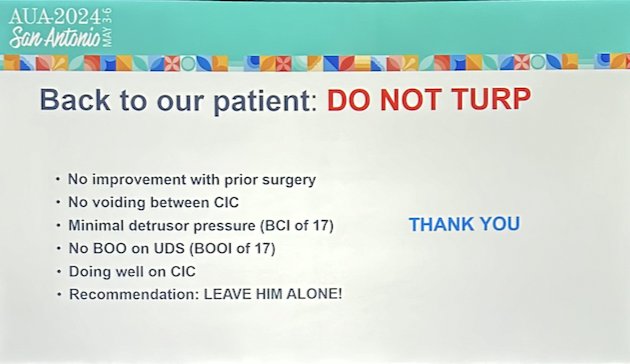
To conclude, Dr. Humphreys once again took the podium to provide some summarizing thoughts, boiling both arguments down to their salient points. He finished the session by taking an audience poll, in which the audience overwhelmingly voted in support of the operative management of the patient. Additionally, the audience similarly voted for operative management if they were the patient in this case, suggesting that if they were the patient, they would like to be given the chance to spontaneously void via TURP procedure.
Presented by:
- Mitchell Humphreys, MD, Mayo Clinic Arizona, Pheonix, AZ
- Nicole Miller, MD, FACS, Vanderbilt University, Nashville, TN
- Ricardo Gonzalez, MD, Houston Methodist Hospital, Houston, TX
- Christopher Tenggardjaja, MD, Kaiser Permanente, Oakland, CA
- Matthew Rutman, MD, Presbyterian Allen Hospital, New York, NY
Written by: Jacob Tsai, BS, LIFT Fellow in the Department of Urology, University of California Irvine, @jacobtsai0918 on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, May 3-6, 2024, San Antonio, Texas


