(UroToday.com) The Sunday morning plenary sessions covered various topics within the field of men’s sexual medicine. In this particular discussion, a decorated panel of men’s health specialists engaged in a panel discussion regarding the tips and tricks for penile prosthesis surgery. The panel was comprised of Dr. Petar Bajic from Cleveland Clinic, Dr. Amy Guise from Froedtert and Medical College of Wisconsin, Dr. Steven Wilson from the Institute for Urologic Excellence, Dr. Charles Welliver from Albany Medical College, Dr. Hossein Sadeghi-Nejad from NYU Langone Grossman School of Medicine, and Dr. Jonathan Clavell Hernandez from Clavell Urology.
The discussion began with Dr. Hossein Sadeghi-Nejad, the moderator of this session. He began by discussing the rarity of the inflatable penile prosthesis procedure, showing SEER data in which only 3 percent of individuals with erectile dysfunction after prostate radiation or extirpation. With this data, he posed that implantation of inflatable penile prostheses is an underutilized procedure, citing multiple reasons. These reasons were separated into patient vs. surgeon specific, citing stigma, awareness, misconceptions, preference for less invasive management, cost and accessibility, and psychological factors for patients. Meanwhile, surgeon issues for underutilization of this procedure included training and skills, complexity, complications, low demand, and psychological factors.
The first topic discussed the implantation of ectopic reservoirs, presented by Dr. Guise. Dr. Guise opened her discussion by talking about the procedural steps of implanting an ectopic reservoir, highlighting the optimal placement submuscularly 6-8 cm into the abdomen in line with the ipsilateral nipple. In this procedure, she describes getting access through the external ring, using the pubic tubercle as a fulcrum to aim anteriorly. She then went on to discuss the complication profile of this procedure, highlighting the increased incidence of herniation after surgery. In patients with higher risks of herniation, she recommended either lower submuscular implantation or trans-fascial high placement, both of which are designed to minimize herniation and migration of the implant.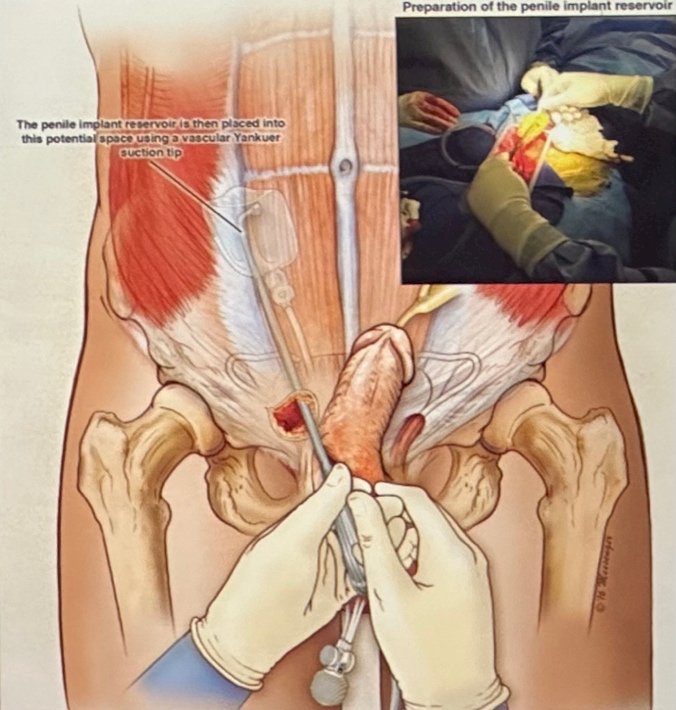
Dr. Guise continued her talk by offering alternative locations of implantation. First, she described implantation into the lateral retroperitoneum, in which the transverse incision is placed 2cm medial and inferior to the anterior superior iliac spine, and blunt puncture into the space of retzius allows for secure implantation. Additionally, she described the implantation via suprapubic incision, which allows for direct visualization and placement into the space of retzius anterior to the bladder. She highlighted how this approach would be beneficial for the patient as they can see their device, as well as for the patient with bilateral inguinal hernia repairs in which access via the inguinal canals would be difficult.
In conclusion, she proposed three summarizing thoughts:
- Ectopic reservoir placement should be utilized for patients desiring an inflatable prosthesis but the space of retzius has been violated.
- High submuscular, lateral retroperitoneum and suprapubic locations are all viable options.
- Submuscular reservoirs have higher risks of herniation and can be palpable, but patient satisfaction remains high.
Dr. Welliver was the next to take the podium, discussing the management of infected implants. He began by highlighting the initial presentation symptoms and signs of these patients, highlighting that this is a clinical diagnosis mostly made on physical exam. While there are subtle signs such as a tethered pump or erythema and calor, more definitive signs of purulence, lack of healing, erosion, or systemic symptoms also typically are present. He then presented the question: Who can you salvage? Dr. Welliver argued that most people should be salvaged, with only absolute contraindications of sepsis and significant tissue necrosis being reasons to not salvage.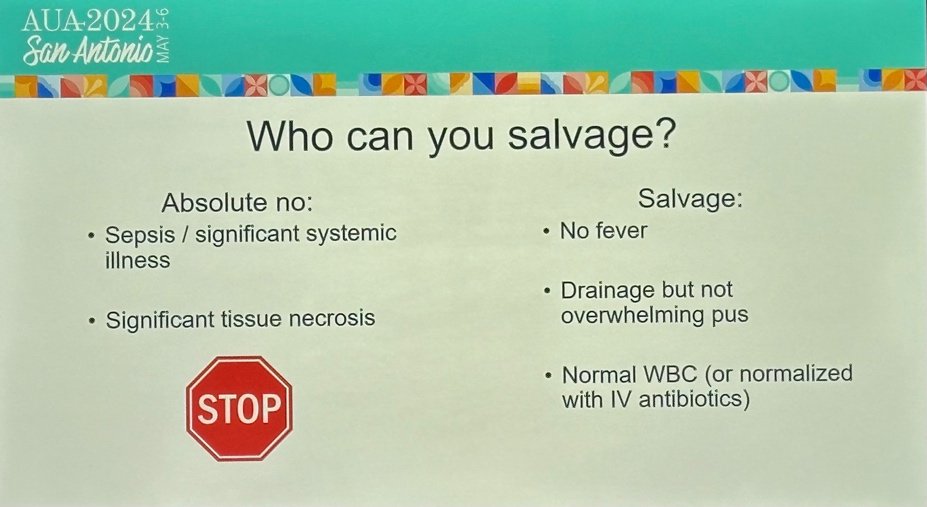
Dr. Welliver continued discussing the initial management of implant infection, discussing the need to stay calm without rushing to explantation, which would result in significant loss of length and girth for the patient. He recommended hospital admission, cultures, and empiric IV antibiotics selected based on the local antibiogram. Dr. Welliver then recommended salvage whenever possible, citing multiple studies that show its efficacy.
Despite the evidence showing the efficacy of salvage, it remains underutilized, being done only about 20% of the time. Dr. Welliver proposed that the 15% decrease in success rate when compared with explantation is outweighed by the minimal length loss and patient ability to remain sexually active with a malleable device. He concluded by reminding everyone that despite most patients being eligible for salvage, few actually receive this course of treatment.
Dr. Bajic took the podium next, presenting on the severe length loss following implant explantation. He presented a 58-year-old diabetic male who had virgin IPP at an outside hospital with a complicated postoperative course due to a device infection. During the removal, the corpora were full of pus and the device was removed, and a salvage procedure was not performed. 1 month later, his diabetes is well controlled, and he is presenting wanting another implant with minimal size loss.
Dr. Bajic then went through considerations for this case, including minimizing length and girth loss, optimal reimplant time, maximal safe implant size, and optimal cosmetic results. To maximize these considerations, Dr. Bajic provided background in the pathophysiology of prosthesis infection and its downstream effects. He discussed how infection results in reduced tunical elasticity, reducing SPL and girth. Simultaneously, infection also causes fibrosis of the cavernosal tissue, resulting in difficult dilation and the need for narrow cylinders. As such, maximizing outcomes revolves around preserving the vascular areas.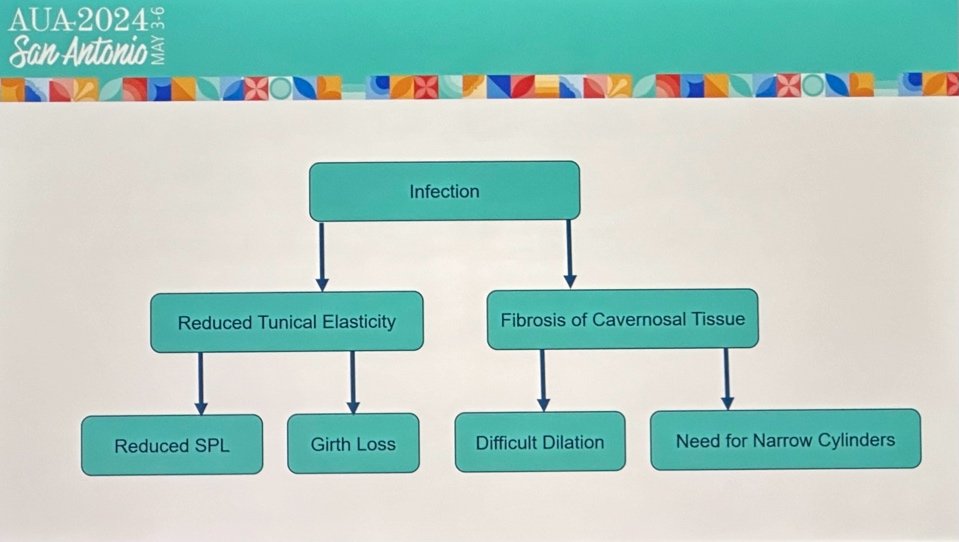
After maximizing vascular preservation during explantation, post-infection rehab can also improve outcomes. Dr. Bajic discussed various modalities of increasing length and maximizing girth post-infection, mentioning both vacuum erection device therapy and penile traction therapy. He presented data showing how vacuum erection device therapy and penile traction therapy have both been shown to increase penile length. To maximize girth, he discussed the technique by which a new IPP can be used as a tissue dilator, which can initially be a narrow cylinder but eventually replaced with a normal or standard cylinder to restore girth. In sum, Dr. Bajic presented multiple modalities to maximize patient satisfaction after infected IPP explantation.
Following Dr. Bajic was Dr. Clavell, who discussed various rerouting procedures for impending erosion. Dr. Clavell began by defining impending erosion as when the cylinder has worked its way against or through a weakened tunica albuginea. Typically, this impending erosion is under the skin in the glans penis and can often be found in combination with other pathologies.
Some of the risk factors that Dr. Clavell discussed included aggressive dilation, chronic mechanical pressure from an oversized cylinder, and placement of the cylinder in a very narrow corporal cavity. Dr. Clavell then detailed 3 cases, the first of which was a patient with a pending erosion but with a working device. He outlined how this procedure would begin with a distal counter incision with subsequent incision of the tunica albuginea and outer wall of the capsule to expose the cylinder. After placing stay sutures, the new corporal space would be dilated and created, allowing for re-insertion of the implant. At this point, he described the placement of a graft that may be placed over the distal edge of the tunica and sewn to the lateral edges. He similarly presented other cases, all of which would subsequently be managed through similar re-routing procedures, just at various locations depending on the site of erosion.
Dr. Wilson was the last presenter, discussing how fibrosis shrinks erectile tissue after IPP placement and infection. He began by detailing how this is the most difficult surgery in prosthetic urology and has the most patient dissatisfaction regardless of the surgeon’s victory in re-insertion. When penile fibrosis occurs, there are multiple methods of surgical management to re-insert the IPP into the scarred corporal body, including multiple incisions with minimal scar excision, extensive corporotomy and graft coverage, extensive corporotomy with excavation of the scar, endoscopic resection of the scar, and lastly the tunnel technique of developing cavernotomes. All these methods were an improvement over the prior traditional method of sharp excision of fibrosis tissue, which gave only 50% chance of success.
After this discussion, Dr. Wilson played a video describing his tunneling technique with the use of specialized cavernatome dilators, which traumatically dilate a new cavern within the corpora in which a cylinder can be placed. He concluded by discussing that despite requirement of an initial narrow cylinder placement, it is feasible to later switch to a regular standard cylinder, with the initial cylinder acting as a fibrotic tissue expander.
Dr. Wilson’s presentation concluded the panel discussion, and Dr. Sadeghi-Nejad closed the plenary session by reviewing each presenters’ key takeaways to wrap up an enthralling panel session.
Presented by:
- Petar Bajic, MD, Cleveland Clinic, Cleveland, OH
- Amy Guise, MD, Froedtert and Medical College of Wisconsin, Milwaukee, WI
- Steven Wilson, MD, FACS, FRCS, Institute for Urologic Excellence, La Quinta, CA
- Charles Welliver, MD, Albany Medical College, Albany, NY
- Hossein Sadeghi-Nejad, MD, FACS, NYU Langone Grossman School of Medicine, New York, NY
- Jonathan Clavell Hernandez, MD, FACS, Clavell Urology, Houston, TX
Written by: Jacob Tsai, BS, LIFT Fellow in the Department of Urology, University of California Irvine, @jacobtsai0918 on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, May 3-6, 2024, San Antonio, Texas


