(UroToday.com) The 2024 American Urological Association (AUA) annual meeting featured a session on testicular cancer, and a presentation by Dr. Julian Chavarriaga discussing a propensity-matched analysis of open versus robotic primary retroperitoneal lymph node dissection (RPLND) for CS II testicular cancer. RPLND remains a primary management option for CS IIA/B and relapsed CSI with IIA/B equivalent disease. Open RPLND has been the gold standard technique for primary RPLND, but is technically challenging with a complication rate in the primary setting of 10-20%. However, the advent of minimally invasive techniques has led to increasing utilization of robotic RPLND due to the potential for lower blood loss, shorter length of stay, faster recovery, and superior cosmetic results. A direct comparison of oncological and perioperative outcomes between these surgical approaches is lacking. High quality data regarding the oncological risks and benefits are needed from well-designed retrospective studies. To address this unmet need, Dr. Chavarriaga performed a propensity matched analysis to limit the impact of selection bias on survival and perioperative outcomes.
This study was a retrospective review of all patients who underwent primary robotic and open RPLND, between 1990 to 2022 at the Princess Margaret Cancer Centre. The authors used a 2:1 (open RPLND : robotic RPLND) propensity score matching analysis (based on age, obesity, clinical stage, retroperitoneal mass size and location, and tumor marker status prior to RPLND) in order to adjust for the effects of inherent differences between patients undergoing open RPLND and robotic RPLND. All surgeries were nerve-sparing bilateral template RPLND and were performed by two experienced testicular cancer surgeons. The primary endpoint was to establish the risk of relapse associated with both surgical approaches. Secondary endpoints included perioperative outcomes such operative time, length of stay, estimated blood loss, need for transfusion, and surgical complications. Relapse free survival rates were calculated using the Kaplan-Meier product-limit method, and log-rank test was used to assess the impact of both surgical approaches.
A total of 178 patients underwent primary RPLND during the study period. Of these patients, 137 underwent open RPLND and 41 underwent robotic RPLND. After propensity score matching, 26 patients were matched in the robotic RPLND and 38 in the open RPLND groups. The distribution showed a good match, with no significant differences between the two groups after matching. The patient characteristics are as follows:

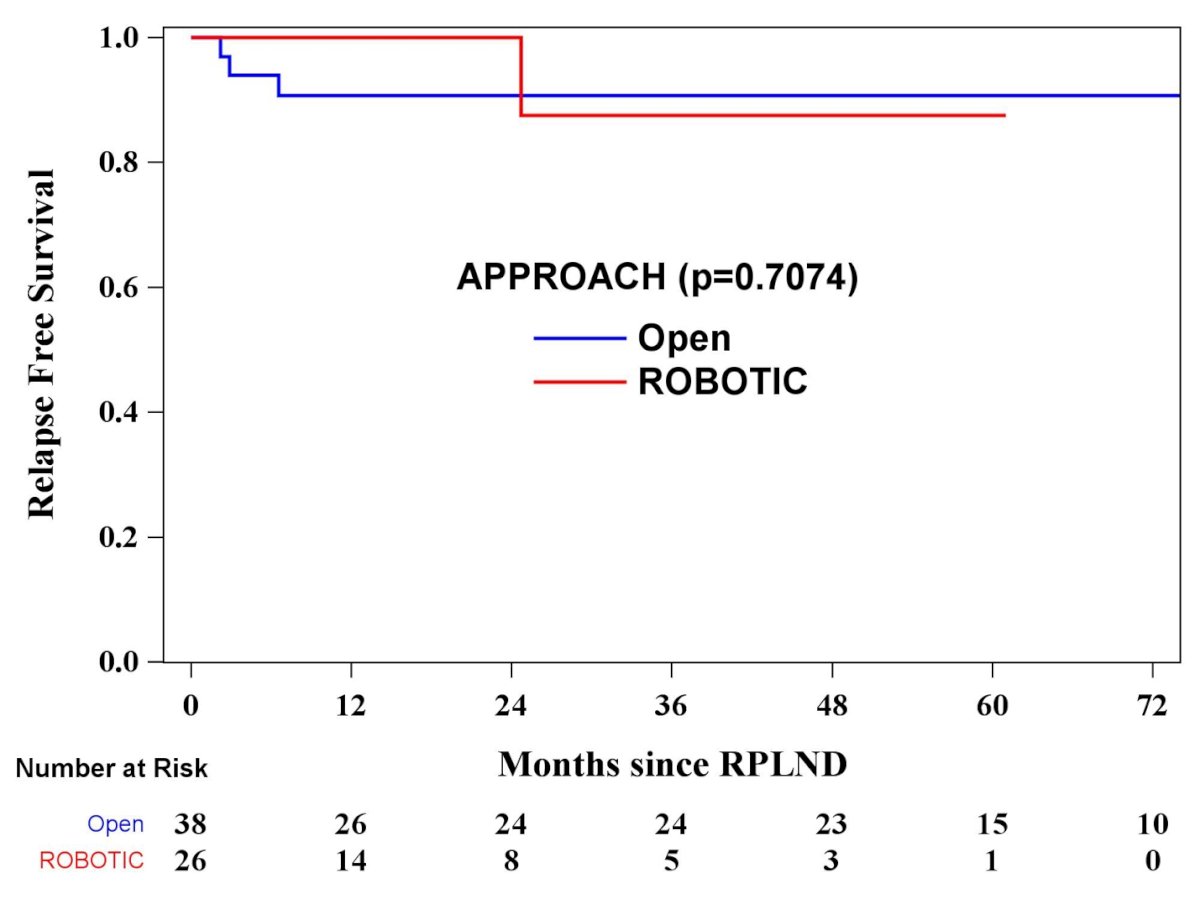
With a median follow-up of 23.6 months (IQR 4.4-59.2) only 1 patient (3.8%) relapsed in the robotic RPLND group versus 3 patients (7.8%) in the open RPLND group, with all relapses being out of field. However, the difference was not statistically significant (p = 0.7074):
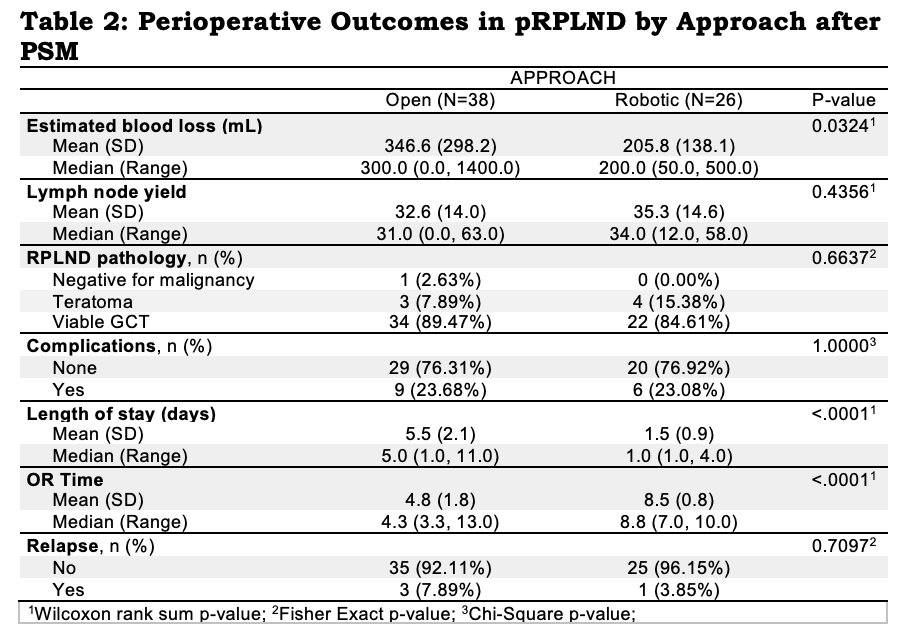
Robotic RPLND was associated with a lower median length of stay (1 vs. 5 days, p<0.0001), and median estimated blood loss (200 vs. 300 ml, p = 0.032). There was no significant difference in the complication rate (24% vs 25%, p = 1.00) or median lymph node yield (34 vs 31 nodes, p = 0.435). However, the median OR time was significantly longer with robotic surgery (8.8 vs. 4.3 hours, p < 0.0001):
Several strengths of this study include the bilateral template approach, single surgeon (for robotic RPLND), all patients being CS II (initial or relapsed CS I), and no adjuvant chemotherapy for pN+. The limitations of this study include: (i) retrospective design with unmeasured confounding variables, (ii) differences in surgical technique through the years, (iii) all surgeons in the present series having significant experience with RPLND, (iv) the learning curve of robotic RPLND, and (v) the small sample size and limited follow-up.
Dr. Chavarriaga concluded his presentation by discussing a propensity-matched analysis of open versus robotic primary retroperitoneal lymph node dissection for CS II testicular cancer with the following take-home messages:
- This is the first study to compare open RPLND and robotic RPLND using a propensity score matching system, allowing it to approximate the results that might be observed in a randomized trial
- Primary robotic RPLND offers low morbidity and improved perioperative outcomes, while maintaining the excellent oncologic efficacy of the open approach
- Primary robotic RPLND should be incorporated into guidelines provided it is carried out by surgeons by high-volume experience in RPLND
Presented by: Julian Chavarriaga, MD, University of Toronto, Toronto, Canada
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, Fri, May 3 – Mon, May 6, 2024.


