(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3 and May 6, 2024, was host to the Upper Tract Transitional Cell Carcinoma podium session. Dr. Francesco Cattafi presented the results of an observational study of Lynch Syndrome among upper tract urothelial carcinoma (UTUC) patients.
Dr. Cattafi started his presentation by saying that Lynch syndrome is a genetically dominant autosomal disease that predisposes individuals who have this syndrome to a broad spectrum of neoplasms, including UTUC, and there is an increased lifetime risk of developing colorectal cancer (80-90%), endometrial cancer (40-60%), ovarian cancer (1-24%) and UTUC (28%). He continued to say that Lynch syndrome has a prevalence of 2-3% of genetic inherited or germline mutations on DNA mismatch repair genes (MLH1, MSH2, MSH6, PMS2, EPCAM). He presented the first results of an outpatient clinic dedicated to treating patients with Lynch syndrome.
From 2021 to 2024 they observed 36 patients with Lynch syndrome. The investigators collected prospectively data regarding Lynch syndrome mutations, and medical and family history and simultaneously started a strict follow-up protocol. Genetic data was obtained both by Immunohistochemistry (IHC) and by next-generation genetic sequencing. They assessed the concordance between Bethesda, EAU guidelines, Amsterdam II criteria, and PREMM 5 score model for Lynch syndrome. Characteristics of the patients are shown in the table 1 below.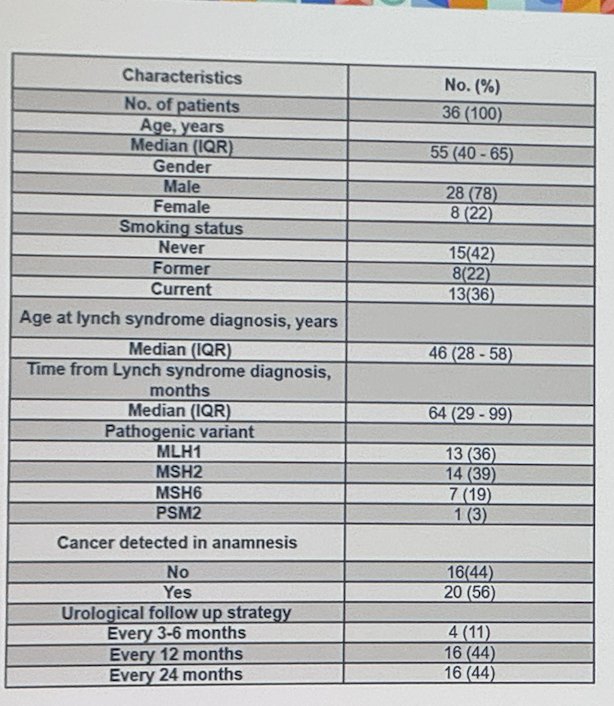
Their Follow-up protocol consisted on:
- Ultrasound (US) every 2 years
- Urinalysis every 2 years
- Urinary cytology every 2 years
*In high-risk cases (age >50 years, MSH2 mutation carriers and family history of UCT scans were alternated with US every year
- Urinary cytology every year
Dr. Cattafi went on to explain that of the 30 patienLynchth lynch syndrome 53% (16 patients) received their Lynch syndrome diagnosis after they had been diagnosed with cancer, while 47% (14 patients) were identified via genetic counseling after degree relative diagnosis. This coLynchof lynch syndrome included 11 colorectal cancer cases (36%), 4 UTUC (13%), and others with endometrial, gastric, and skin cancer. The lifetime risk of cancer varied according to the MMR mutation they had (MLH1, MSH2, MSH6/PSM2)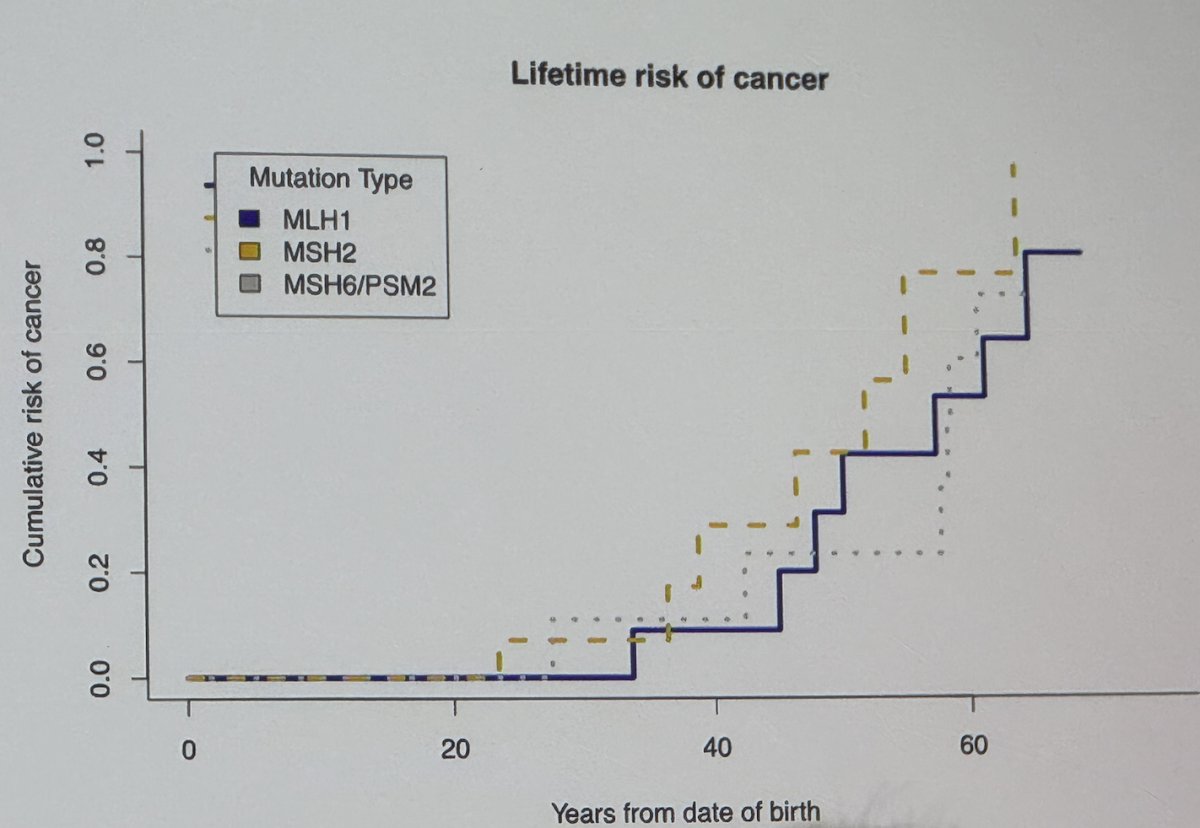
MSH2 mutations were the most common mutations overall, followed by MLH1 mutations in the second place. MSH2 mutation was detected in half of the patients with UTUC (50%) and were also commonly detected in patients with colorectal cancer (36%).
The median age at diagnosis of UTUC was 61 years, which exceeded that of colorectal cancer (49 years, p=0.007). The lifetime risk of cancer varied according to site and the most incident one was colon, followed by endometrial, lung, pancreas, stomach, and UTUC.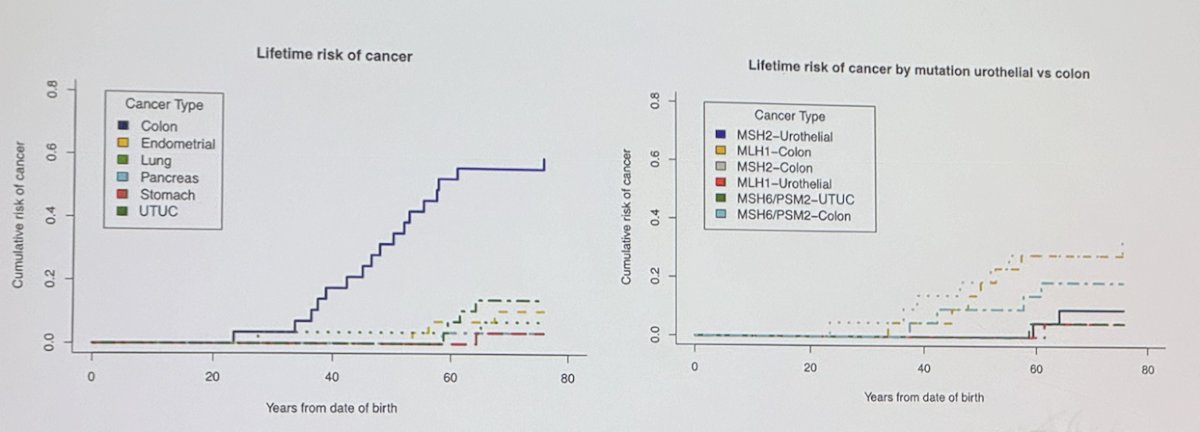
In diagnosing Lynch syndrome, Bethesda and EAU guidelines (if >65 years of age) demonstrated greater accuracy (83% and 100%, respectively) compared to Amsterdam II criteria (56%). The PREMM 5 (94% accuracy) score outperformed most of the models.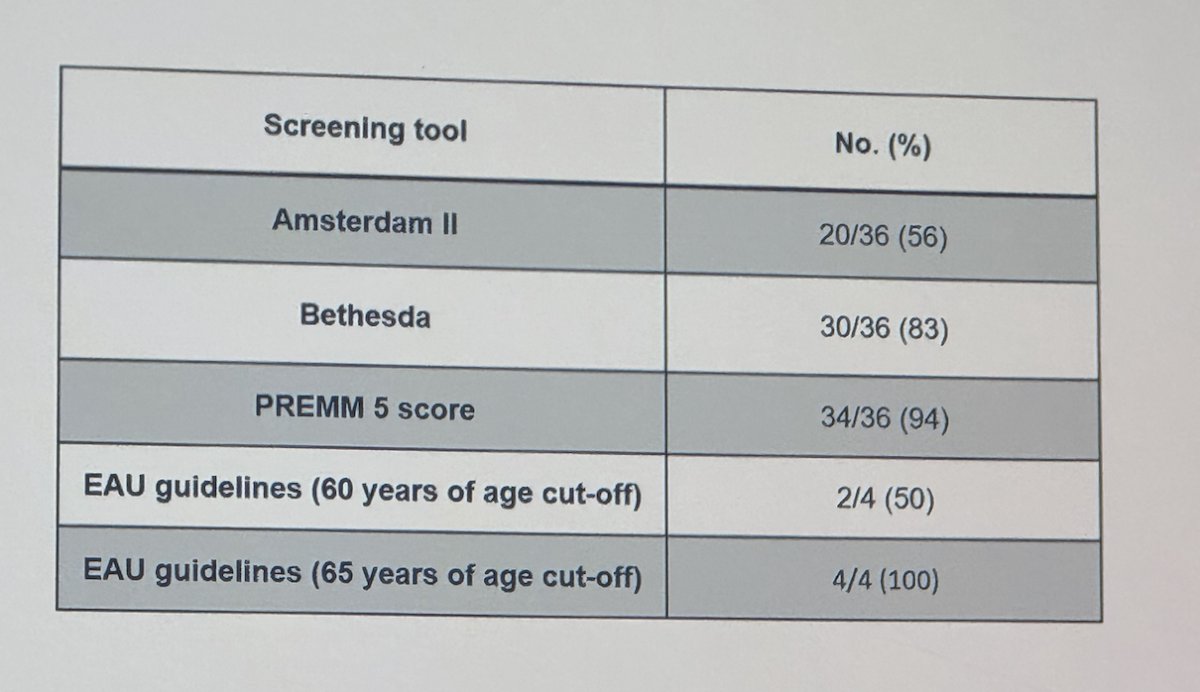
They tailored their follow-up protocol based on the identified MMR gene mutation, please refer to the table below.: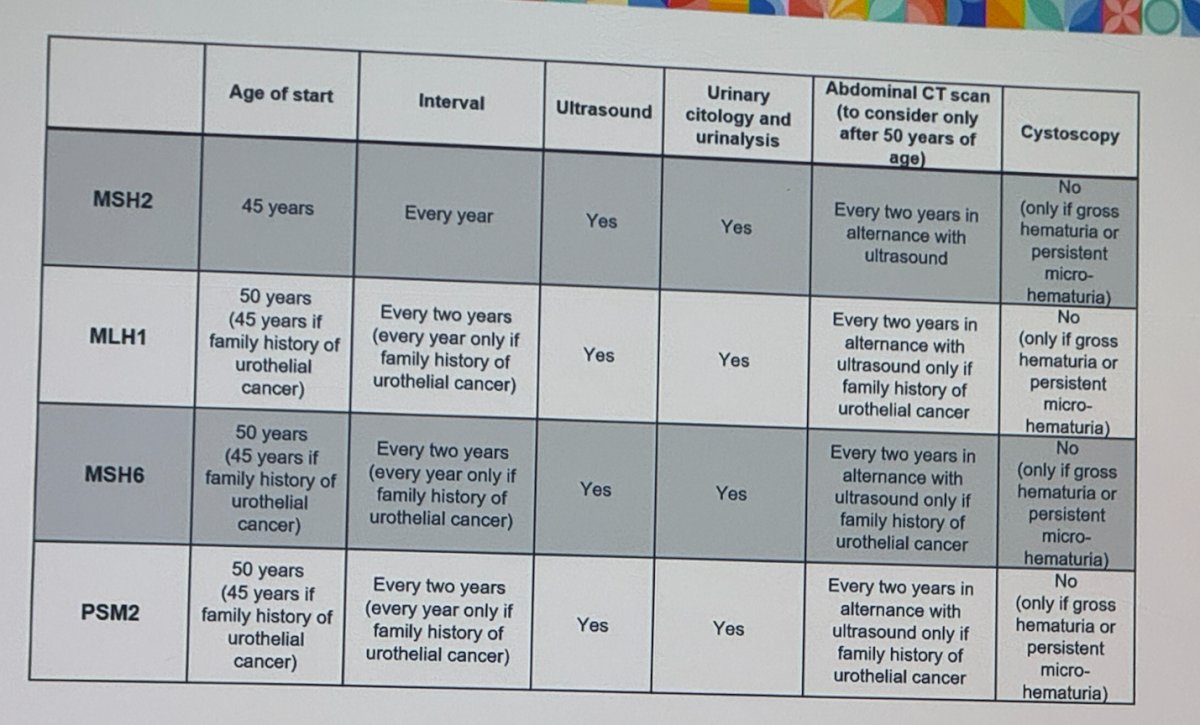
Dr. Cattafi concluded his presentation by delving into the incidence of upper tract urothelial carcinoma and mutational patterns observed during urological follow-ups of Lynch Syndrome patients. He highlighted the establishment of a specialized Lynch Syndrome clinic over the last three years, which has provided significant insights into prevalent mutations. This development holds promise in crafting mutation-specific follow-up protocols and improving early detection of upper tract urothelial carcinoma among this particular population. Their next steps involve validating the PREMM 5 model in 25 patients with UTUC and determining whether NGS genetic testing is necessary when the PREMM 5 score suggests Lynch syndrome.
Presented by: Francesco Cattafi, MD, Postdoctoral Researcher, IRCCS Ospedale San Raffaele, Milan, Italy
Written by: Julian Chavarriaga, MD - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX between May 3rd and May 6th, 2024


