(UroToday.com) The 2024 American Urological Association (AUA) annual meeting held in San Antonio, TX was host to the Society of Urologic Oncology (SUO) session Dr. Phillip Pierorazio debated against lymph node dissection for Upper Tract urothelial carcinoma.
Dr. Pierorazio began his talk by stating that it is challenging to argue against lymph node dissection for upper tract urothelial carcinoma (UTUC), given that three international clinical practice guidelines recommend it. He then discussed that the National Comprehensive Cancer Network (NCCN) recommends regional lymph node dissection if tumors are high grade, while the European Association of Urology (EAU) suggests templated-based lymph node dissection for all patients scheduled for right nephroureterectomy due to high-risk UTUC, and also the AUA/SUO guideline recommends that for patients with high-grade UTUC physicians should perform lymph node dissection at the time of resection, and for low-grade UTUC they may consider it.
He then proceeded to discuss the considerations for lymph node dissection in UTUC. Firstly, we must determine if lymph node dissection offers a staging benefit or a therapeutic benefit, both at the expense of the risks of an additional procedure. He acknowledged that data regarding lymph node dissection in UTUC is limited, and one of the main reasons for this is the insufficient number of lymph node dissections performed.
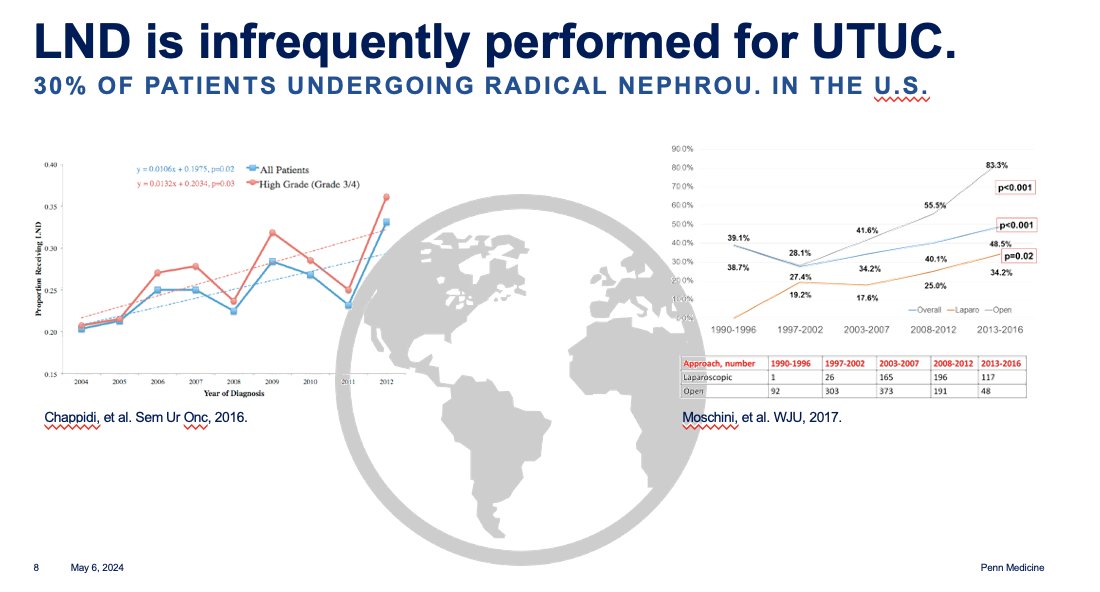
Dr. Pierorazio presented data from the United States (U.S.) indicating that only 30% of patients undergoing radical nephroureterectomy undergo lymph node dissection.
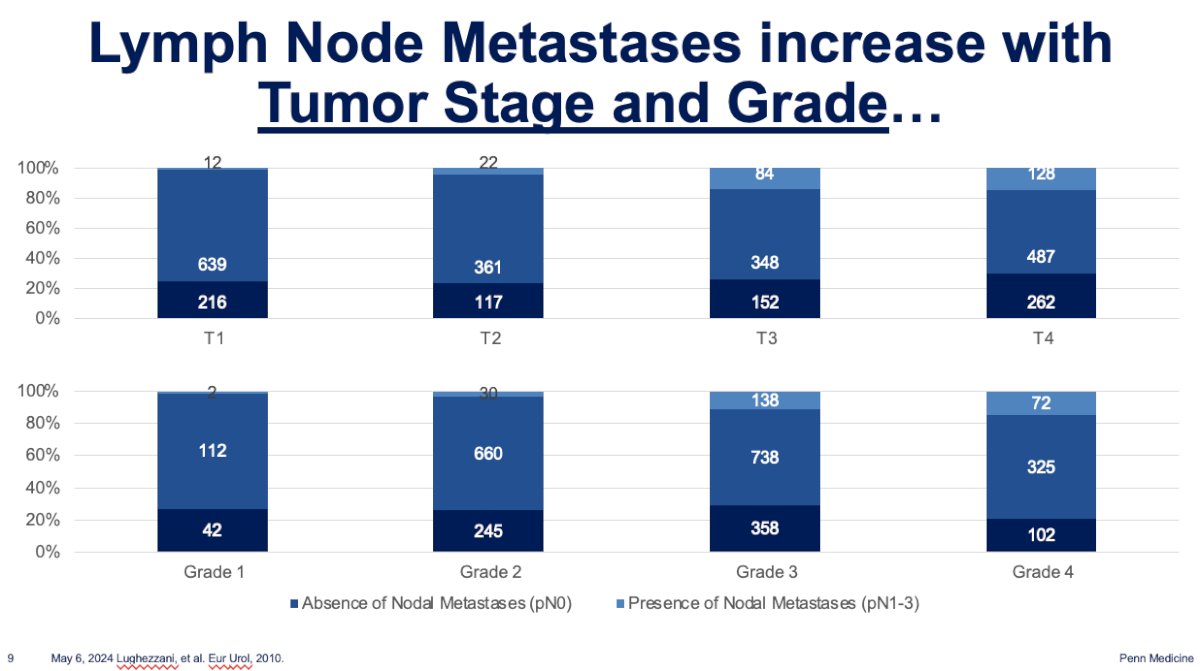
Additionally, the incidence of node-positive (N+) disease among patients with UTUC is low, and it varies significantly based on the T stage (p<0.001) and tumor grade (p=0.002). Dr. Pierorazio discussed findings from a large retrospective cohort study of UTUC patients reported by Lughezzani et al. They observed that after lymph node dissection, only 1.4% of patients with T1 stage had N+ disease, compared to 14.2% among those with T4 disease. Similarly, for patients with Grade 1 UTUC, 1.3% had N+ disease compared to 14.4% among Grade 4 patients.1 Please refer to the table below.
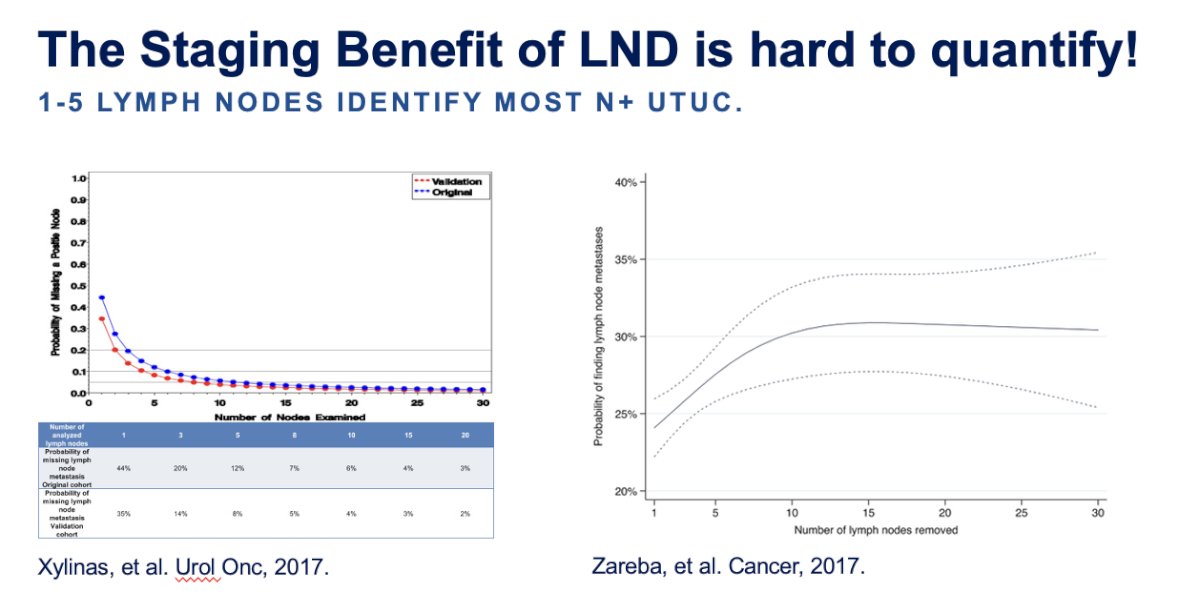
Dr. Pierorazio noted that quantifying the staging benefit of lymph node dissection is challenging, and the extent of lymph node dissection remains uncertain, as N+ UTUC is typically identified in only 1-5 nodes. He presented two studies demonstrating that harvesting a greater number of lymph nodes decreases the likelihood of missing lymph node metastasis. However, this effect is not observed when harvesting more than 10 lymph nodes in either study.2,3
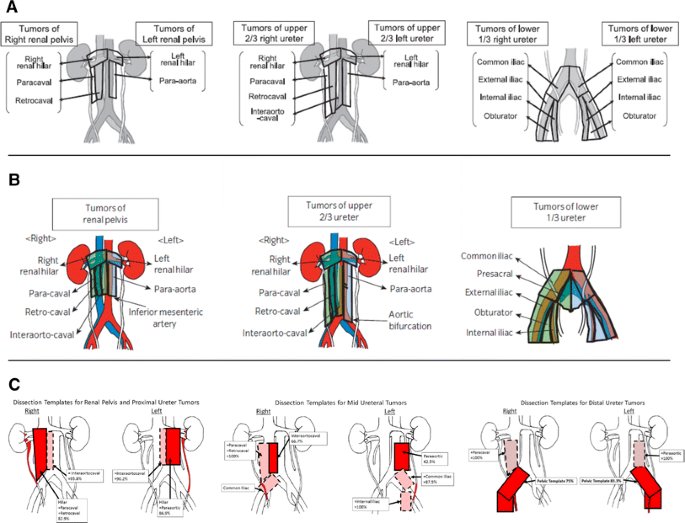
The templates for lymph node dissection for UTUC have varied significantly among different retrospective studies. Dr. Pierorazio discussed the various templates and landing zones of lymph node metastasis, which are typically utilized depending on the tumor's location. For instance, he noted that for tumors of the right renal pelvis, the lymph node landing zones commonly include the right renal hilar, paracaval, and retrocaval regions. Similarly, for tumors involving the upper two-thirds of the right ureter, these landing zones remain the same, but also encompass the interaortocaval area. On the other hand, tumors of the lower third of the right ureter often involve the common iliac, external iliac, internal iliac, and obturator nodes as landing zones. Dr. Pierorazio emphasized the importance of adhering to these templates when performing lymph node dissection as they were designed based on the most common landing zones for UTUC. The templates are outlined below:
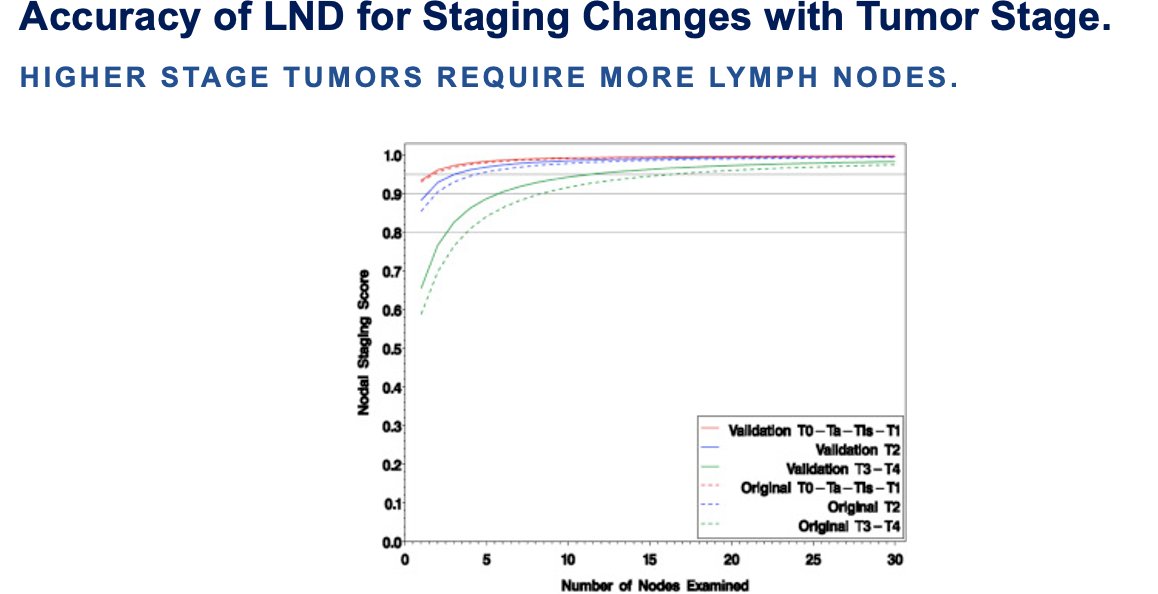
Furthermore, he emphasized that it's not solely about templates or the number of lymph nodes resected, but also about the accuracy of lymph node dissection for staging, which varies with tumor stage.3 Dr. Pierorazio underscored the importance of tailoring lymph node dissection according to tumor stage. He cited a study by Xylinas et al. which confirmed that higher stage tumors require harvesting more lymph nodes for staging purposes.
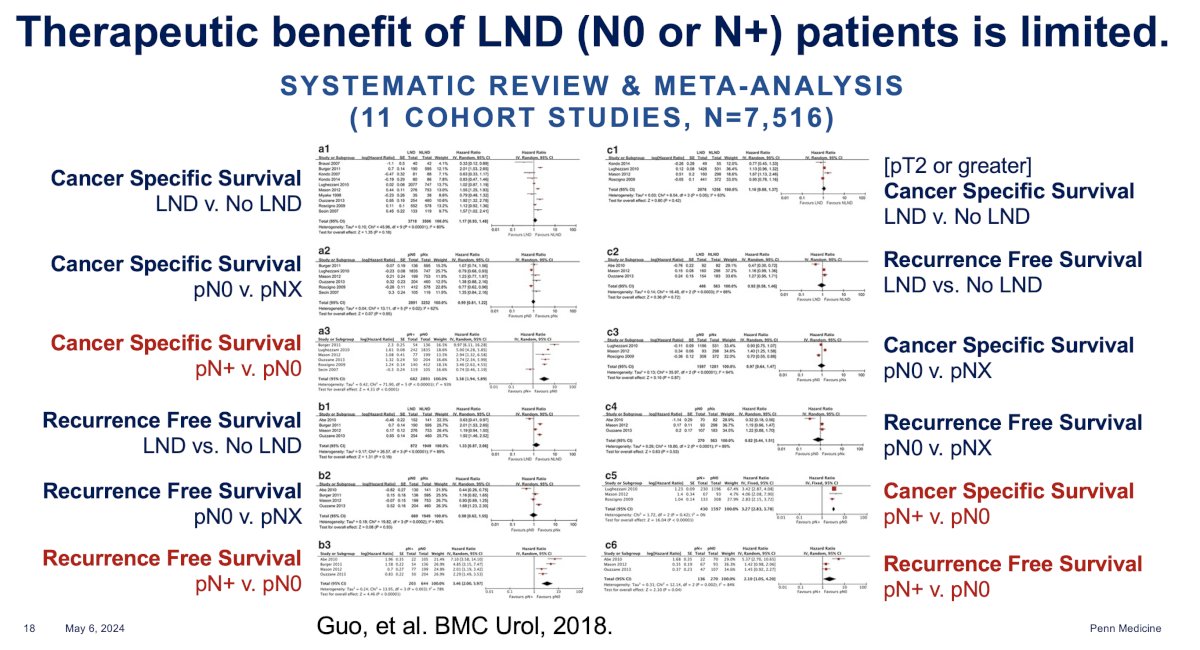
Dr. Pierorazio discussed the poor survival outcomes for patients with node-positive UTUC and questioned the therapeutic benefit associated with lymph node dissection. He presented a systematic review and meta-analysis involving over 7,516 patients with UTUC. This study revealed that for all UTUC patients or those with pT2 or greater tumors, the presence of N+ disease correlated with worse cancer-specific survival and recurrence-free survival. However, among the overall population with UTUC and pT2 or greater tumors, no differences in recurrence-free or cancer-specific survival were observed between patients who underwent lymph node dissection compared to those who did not.
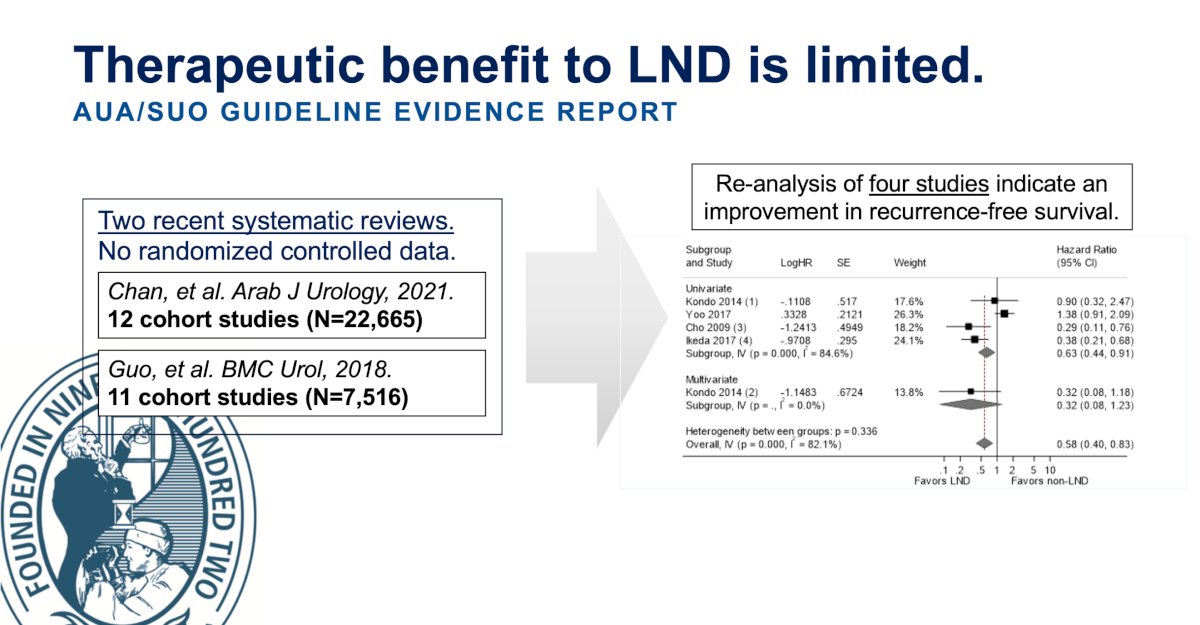
The AUA/SUO guideline incorporated two recent systematic reviews, initially lacking randomized controlled data. Both studies concluded that there were no statistically significant differences in oncologic outcomes, even among higher stage tumors. However, the AUA/SUO panel conducted a re-analysis of four studies, indicating an improvement in recurrence-free survival.
Another argument against lymph node dissection for UTUC is the challenge of quantifying its therapeutic benefit. For instance, in the POUT trial4 which compared adjuvant gemcitabine and platinum-based chemotherapy, subgroup analysis revealed no benefit of adjuvant chemotherapy compared to surveillance in patients with N+ disease (who had undergone a lymph node dissection), in terms of disease-free and overall survival (Figure below). This adds to the point that with more effective systemic therapy, assessing the therapeutic benefit of lymph node dissection becomes increasingly difficult.

Dr. Pierorazio then delved into the feasibility and safety of lymph node dissection for UTUC. He noted that complications during or after robot-assisted nephroureterectomy range between 15-45%, which could potentially be attributed to lymph node dissection (including chylous ascites, vascular injuries, and pancreas injury).
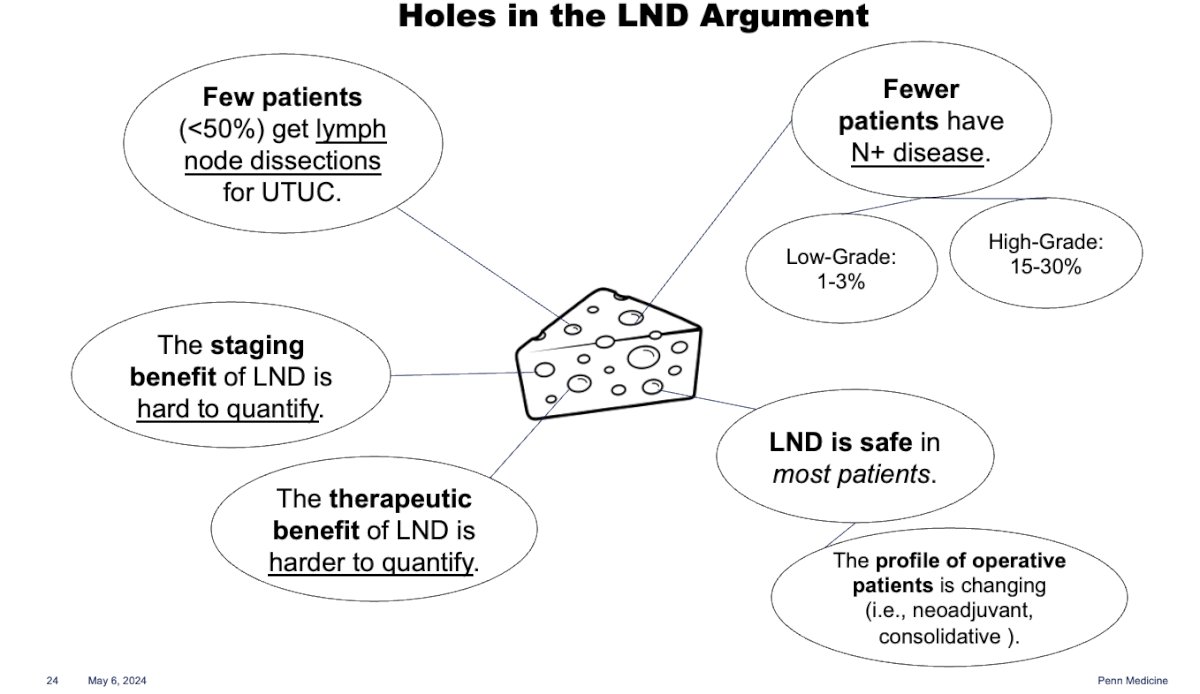
He summarized the gaps in the lymph node dissection argument nicely using the graphic below. In essence, the limited number of lymph node dissections for UTUC, coupled with the unclear and challenging quantification of staging and therapeutic benefits, along with the low number of patients with N+ disease, pose significant challenges. Furthermore, the availability of multiple options for adjuvant therapy, which were previously unavailable, now influences the survival and prognosis of UTUC.
Dr. Pierorazio concluded his presentation with impactful key takeaway messages:
- We need to do more lymph node dissections for UTUC
- With more and better data, we will be able to quantify both the staging and therapeutic benefit of LND for UTUC (Although harder in the era of adjuvant immunotherapy and chemotherapy)
- Consider avoiding a LND in patients with certainty if:
- Low-grade and/or non-invasive disease.
- Metastatic disease or nodal disease outside of the primary landing zone (pN2 or greater).
Presented by: Phillip Pierorazio, MD. Urologic Oncologist at the University of Pennsylvania
Written by: Julian Chavarriaga, MD – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @chavarriagaj on Twitter during the 2024 American Urological Association (AUA) Annual Meeting, San Antonio, TX, May 3rd - 6th, 2024
References
- Lughezzani G, Burger M, Margulis V, Matin SF, Novara G, Roupret M, Shariat SF, Wood CG, Zigeuner R. Prognostic factors in upper urinary tract urothelial carcinomas: a comprehensive review of the current literature. Eur Urol. 2012 Jul;62(1):100-14. doi: 10.1016/j.eururo.2012.02.030. Epub 2012 Feb 23. PMID: 22381168.\
- Zareba P, Rosenzweig B, Winer AG, Coleman JA. Association between lymph node yield and survival among patients undergoing radical nephroureterectomy for urothelial carcinoma of the upper tract. Cancer. 2017 May 15;123(10):1741-1750. doi: 10.1002/cncr.30516. Epub 2017 Feb 2. PMID: 28152158; PMCID: PMC5419853.
- Xylinas E, Kluth L, Rieken M, Rouprêt M, Al Hussein Al Awamlh B, Clozel T, Sun M, Karakiewicz PI, Gonen M, Shariat SF. External validation of the pathological nodal staging score in upper tract urothelial carcinoma: A population-based study. Urol Oncol. 2017 Jan;35(1):33.e21-33.e26. doi: 10.1016/j.urolonc.2016.07.022. Epub 2016 Nov 3. PMID: 27816402; PMCID: PMC5576549.
- Birtle A, Johnson M, Chester J, Jones R, Dolling D, Bryan RT, Harris C, Winterbottom A, Blacker A, Catto JWF, Chakraborti P, Donovan JL, Elliott PA, French A, Jagdev S, Jenkins B, Keeley FX Jr, Kockelbergh R, Powles T, Wagstaff J, Wilson C, Todd R, Lewis R, Hall E. Adjuvant chemotherapy in upper tract urothelial carcinoma (the POUT trial): a phase 3, open-label, randomised controlled trial. Lancet. 2020 Apr 18;395(10232):1268-1277. doi: 10.1016/S0140-6736(20)30415-3. Epub 2020 Mar 5. PMID: 32145825; PMCID: PMC7181180.


