(UroToday.com) In anticipation of the 2021 American Urological Association (AUA) Annual Meeting which is being held, in a delayed fashion, in September, the AUA hosted a “May Kick-Off Weekend” which highlighted a variety of important topics in both benign urology and urologic oncology. Saturday afternoon, Adam Feldman led a course entitled “Trimodality Therapy (TMT) for Management of Muscle Invasive Bladder Cancer” along with faculty Richard Lee and Jason Efstathiou.
Following talks that highlighted the rationale for TMT along with radiotherapy and chemotherapy considerations for its use, Dr. Feldman then discussed surveillance following TMT and management of TMT failures.
Dr. Feldman began by emphasizing that cystoscopic surveillance is critical to ensure that there is no local recurrence or persistence of disease. He advocated for operative TURBT biopsies at 2-3 months following treatment. Notably, he emphasized that one should expect eschar and ulceration at the site which can be debrided with a cold loop prior to biopsy. While historically, a second biopsy was performed at 3 months, many are now moving away from this to solely rely on office-based cystoscopic assessment if the initial biopsy is negative. In either case, surveillance continues in much the same way as for high-risk non-muscle-invasive bladder cancer with quarterly evaluation for 1 year, every 4-month evaluation for a subsequent year, bi-annual evaluation until year five, and the annual evaluation for life. This is complemented by voided urine cytology and upper tract surveillance, ideally using CT urography if renal function allows.
He mentioned that, while radiation cystitis is not uncommon, the majority are clinically insignificant and only 5 of 475 patients in the MGH cohort have required cystectomy due to end-stage bladder from radiotherapy.
Dr. Feldman then discussed the management of local recurrences. Utilizing pooled data from the RTOG trials, 10-year rates of recurrence are approximately 36% for non-muscle invasive disease and 14% for muscle-invasive disease.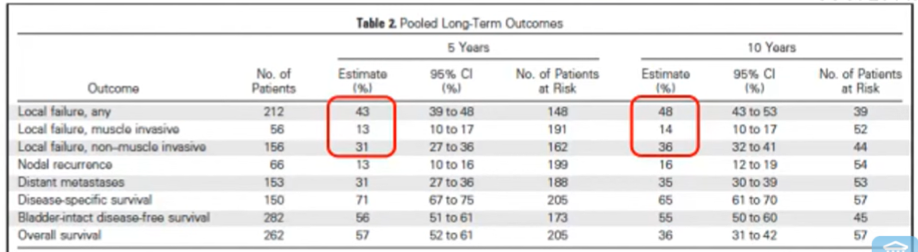
In the MGH cohort, rates were generally similar with a relatively high portion of patients with NMIBC at the time of recurrence having CIS (60%) with 28% having T1 disease and 12% have Ta disease. Rates were generally similar, though slightly lower, in the Erlangen cohort, likely attributable to lower risk disease (including NMIBC) at the time of study accrual.
Utilizing the data from Princess Margaret Cancer Center in Toronto, he emphasized that local recurrence following TMT was more common in patients with larger primary tumors and those with concomitant CIS. This finding was corroborated in the MGH cohort. At MGH, the majority of patients with NIMBC at the time of recurrence were managed with TURBT with or without intravesical therapy. In particular, the majority (74%) received BCG induction following TURBT for NMIBC recurrence after TMT.
In managing non-invasive recurrences, Dr. Feldman highlighted that most can be managed similarly to de novo NMIBC with resection and intravesical therapy. However, timely salvage cystectomy should be offered for those with adverse features including T1 disease, tumor size > 3cm, CIS, or lymphovascular invasion.
Dr. Feldman then transitioned to discussing the management of muscle-invasive recurrences. These should be treated with salvage cystectomy with or without perioperative chemotherapy. In long-term follow-up of the MGH cohort, he highlighted that the overall need for salvage cystectomy was 29% at 5-years and 31% at 10-years. Overall ,13.5% of the cohort underwent salvage cystectomy as a result of recurrent disease found on surveillance. The five- and ten-year survival following salvage cystectomy compare generally quite favorably to those with upfront cystectomy. Other cohort have cited a similar rate of salvage cystectomy.
He then addressed concerns regarding the morbidity of salvage cystectomy. Again relying on the MGH experience, he highlighted 90-day complication rates of 69% overall and 16% major complication rates. These are only marginally higher than complication rates reported from Memorial Sloan Kettering in their series of upfront cystectomies of 64% overall and 13% major. However, it was notable that cardiovascular and hematologic complications (including PE, MI, DVT, and transfusion) were more common in patients undergoing immediate cystectomy following TMT failure, an effect he attributed to the recent chemotherapy which tissue healing complications (including wound, anastomoses, and stomal-related issues) were more common in patients undergoing delayed cystectomy, potentially as a result of the microvascular effects of radiotherapy. A recent direct comparison from MGH examining salvage cystectomy following TMT, primary cystectomy, or primary cystectomy following radiotherapy for another pelvic malignancy (prostate, rectal/anal, or gynecologic) demonstrated no difference in intraoperative or early complications but higher rates of late infectious, gastrointestinal, and genitourinary complications for those undergoing salvage cystectomy following TMT.
In summary, Dr. Feldman highlighted that salvage cystectomy following TMT is associate with a slightly higher complication rate than upfront cystectomy. Furthermost patients will receive ileal conduit or continent cutaneous reservoirs for urinary diversion though neobladders are not impossible, just associated with higher risks of stricture and incontinence.
Presented by: Adam Feldman, MD, MPH, Urologist, Urologic Oncologist, Director, Combined Harvard Urologic Oncology Fellowship, Massachusetts General Hospital
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter during the AUA2021 May Kick-off Weekend May 21-23


