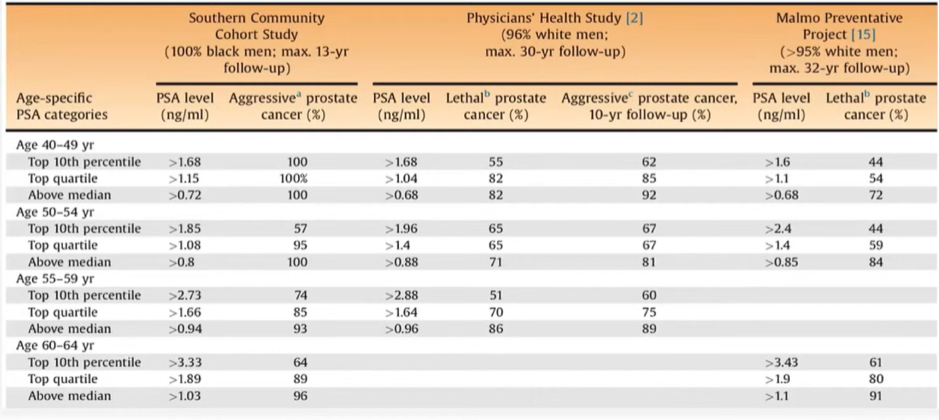
Following an introduction to genomic testing by Dr. Wagner, Dr. Cooperberg discussed the role of pre-diagnostic markers. In this context, he first emphasized that prostate-specific antigen (PSA) is, despite all the controversy, one of the best cancer markers ever discovered. However, it hasn’t been appropriately or optimally used. Further, Dr. Cooperberg advocated for use of early “baseline” PSA testing prior to the development of BPH to provide baseline risk stratification.
In that context, Dr. Cooperberg then highlighted that thee are “more biomarkers than we know what to do with” including not just traditional genomic tests using tissue, blood, and urine, but also advanced imaging approaches which, when used in this disease space, overlaps as a risk stratification approach.

When critically considering the available tests, Dr. Cooperberg emphasized that any candidate marker cannot just have the predictive ability on its own, but must improve on an existing multivariable risk calculator built on clinical characteristics. Further, a high-quality methodology, informed by the REporting of tumor MARKer (REMARK) guidelines and Prospective-specimen collection, Retrospective Blinded Evaluation (PROBE) principle. Finally, the goal of any genomic test should be to detect not just prostate cancer in general, but a clinically significant disease which is potentially lethal.
When examining tests that may be considered prior to a first prostate biopsy, Dr. Cooperberg highlighted PCA2, MiPS, 4K, phi, SelectMDx, ExoDx, and mpMRI may be considered.
PCA3, an mRNA detectable in urine following digital rectal examination, has improved specificity for prostate cancer over PSA though is somewhat less consistent as a predictor for high-grade disease and has more recently fallen out of favor. Operationalized clinically, PCA3 functions best as a two threshold test with low levels having a high negative predictive value and high values having a high positive predictive value but the interpretation of intermediate values being somewhat difficult to interpret.
Both 4K and phi are blood-based tests PSA isoforms with somewhat increased specificity for high-grade disease. The 4Kscore incorporates clinical data including age, digital rectal examination findings, family history and race while phi does not include clinical data. The available prospective comparison of these two tests found that, overall, they performed similarly.
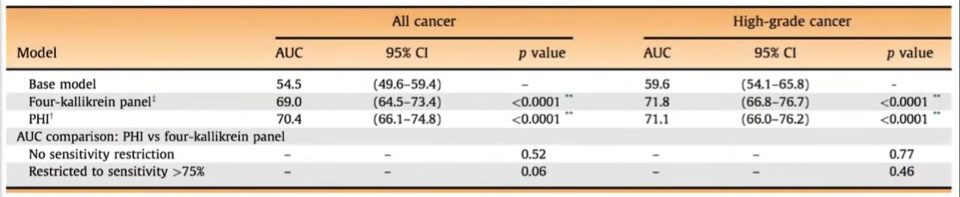
Dr. Cooperberg highlighted that, at UCSF, they use 4K more given that it includes other clinical factors and may have more actionable results.
He then discussed SelectMDx, a more recent, urine-based test. As with PCA3, SelectMDx requires DRE prior to test. Notably, this test has been calibrated for very high negative predictive value with the goal to confidently exclude high-grade disease and avoid biopsy. Another urine-based test, ExoDX, has the advantage of not requiring a digital rectal examination given that it examines exosomal RNA. Thus, it can be performed at home by the patient without clinician involvement which has proven beneficial over the past year in the context of the COVID-19 pandemic. As with SelectMDx, ExoDX is calibrated to predict and ideally exclude high-grade disease.
Apart from the aforementioned comparison of 4K and phi, there are few head-to-head comparisons and Dr. Cooperberg described this as a “dealer's choice”. However, he further highlighted that, for many clinicians and in some jurisdictions, mpMRI is in the same space as a reflex test. Unlike some of the aforementioned genomic tests, he emphasized that the negative predictive value of mpMRI for high-grade disease is not particularly high. Thus, we cannot confidently exclude high-grade disease and omit biopsy.
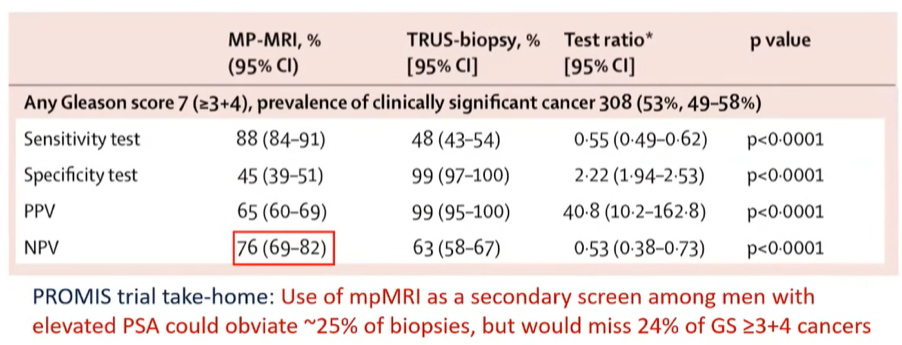
In addition, unlike genomic tests which are rigidly standardized and objective, there is substantial interobserver variability, even among centers of excellence. Thus, in his view, mpMRI should augment but not replace systematic biopsy and doesn’t therefore necessarily perform the same function as the genomic tests described above.
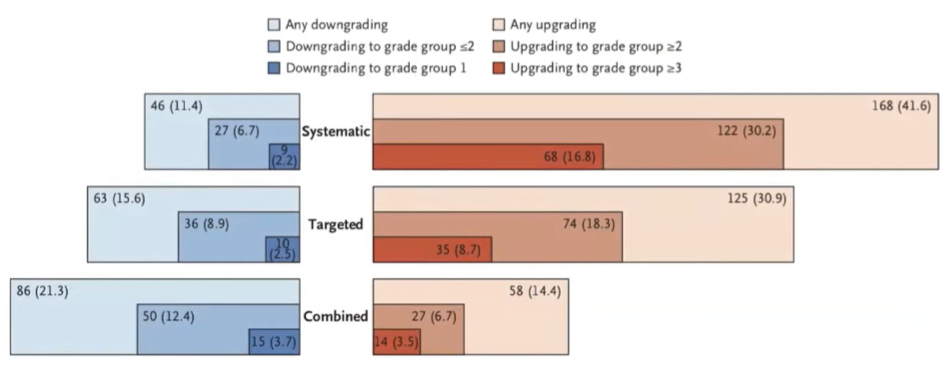
In addition, he emphasized the importance of transrectal ultrasound as a diagnostic approach.
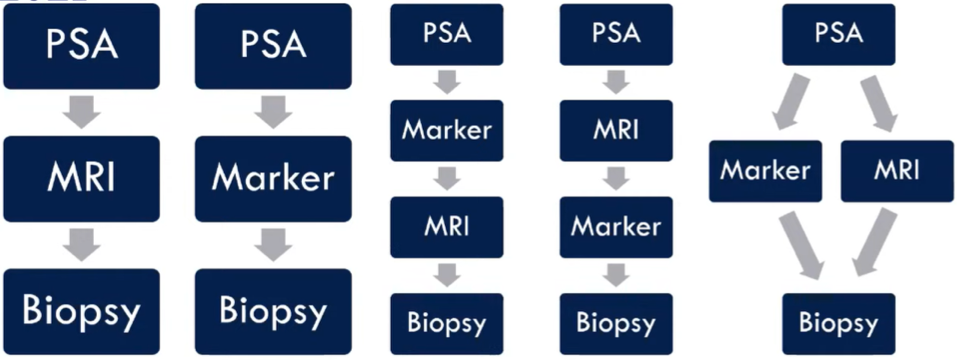
However, he emphasized that we must understand that no prostate cancer test provides a binary outcome, instead it provides risk stratification which needs to be interpreted within the relevant clinical context. Considering how and when to apply these tests, he presented a number of potential models incorporating initial PSA testing, genomic markers, and mpMRI imaging prior to biopsy. In his view, there is rationale to support each of these, though the third option is the one most commonly employed in his practice at UCSF. To do so requires the input and engagement of primary care teams to utilize a reflex genomic marker for risk stratification in patients with abnormal PSA.
In conclusion, he emphasized that optimal PSA screening includes early baseline testing followed by long intervals between testing. Further, we should utilize low PSA threshold for further work-up to minimize under-diagnosis while utilizing secondary tests prior to biopsy to decrease the morbidity of screening programs.
Presented by: Matthew R. Cooperberg, MD, MPH, Professor of Urology; Epidemiology & Biostatistics, Helen Diller Family Chair in Urology, University of California, San Francisco, UCSF
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter during the AUA2021 May Kick-off Weekend May 21-23


