(UroToday.com) The 2021 American Urological Association (AUA) Summer School session on Upper Tract Urothelial Carcinoma included a case-based discussion led by moderator Dr. Surena Matin who was joined by panelists Dr. Sima Porten and Dr. Vitaly Margulis. This case highlighted the diagnosis and treatment of upper tract urothelial carcinoma in patients with suspicion for hereditary disease. This patient was a 56-year-old female with gross hematuria and flank pain with no medical history and a surgical history consistent with a hysterectomy in 1998 and two C-sections. Her family history was negative for genitourinary malignancy, however, her father, sister, and paternal uncle had colon cancer and her father had skin cancer. Physical examination was unremarkable, however, a CT scan demonstrated a 3 cm right distal ureteral mass with hydronephrosis. Cystoscopy and right ureteroscopy showed no bladder tumors, but a bulky low-grade appearing tumor in the distal ureter and no tumors in the proximal ureter and renal pelvis:
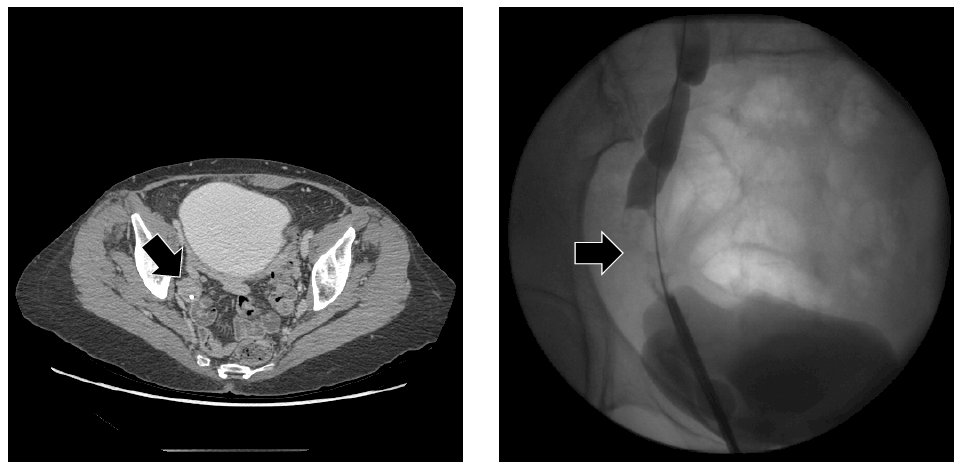
A biopsy of this lesion demonstrated predominantly low-grade papillary urothelial carcinoma with focal high-grade areas, with no definitive stromal invasion identified and no muscularis propria identified. Given the patient’s upper tract urothelial carcinoma diagnosis and her family history as noted, the suspicion for Lynch Syndrome is high. The urinary tract is the third most common organ site affected by Lynch Syndrome as depicted in the following figure:1

Based on predictive nomograms2,3 this patient has a 33% risk of non-organ confined disease and 5-year recurrence-free survival for high-grade disease of ~83%. The best way to screen for Lynch Syndrome is to utilize the Amsterdam 2 clinical “3-2-1” criteria:
- 3 successive generations with Lynch Syndrome-related cancer
- 2 that are first degree relatives
- 1 diagnosed before the age of 50
With regards to tissue testing, a biopsy from the ureteroscopy or nephroureterectomy should be sent for immunohistochemistry by pathology and stains should show positive for four DNA mismatch repair proteins (MLH1, MSH2, MSH6, PMS2). The absence of one or more of these proteins indicates probable Lynch Syndrome. Alternatively, a specimen from the ureteroscopy or nephroureterectomy can be sent for MSI testing via PCR but does require some normal tissue and much more tumor tissue than for immunohistochemistry. The results from PCR will show MSI-stable, MSI-low, or MSI-high, with MSI-high suggesting Lynch Syndrome. Dr. Matin highlighted that if there is a high clinical suspicion, it is always best to refer the patient to a genetic counselor for consideration of germline testing.
Given the patient is cTxcN0 with high grade papillary distal ureteral tumor with hydronephrosis and a 33% risk of non-organ confined disease with an ~83% relapse-free probability, Dr. Matin posed the following treatment options to the panel:
- Endoscopic management
- Nephroureterectomy +/- lymphadenectomy
- Distal ureterectomy, ureteral reimplant, +/- lymphadenectomy
- Neoadjuvant chemotherapy followed by surgery +/- lymphadenectomy
Dr. Margulis notes that it is critical to have an assessment of the function of the kidney given that if it is a poorly functioning kidney there is less of a role/no role for a distal ureterectomy. With a good functioning kidney for this patient, he would consider a distal ureterectomy with a good lymph node dissection and gauge the necessity of additional treatment based on the final pathology, which Dr. Porten agreed with.
The immunohistochemistry from the patient’s ureteral biopsy showed an absence of MSH2 and MSH6 proteins, but germline testing confirmed Lynch syndrome. She eventually underwent a distal ureterectomy with a Psoas hitch ureteral reimplant and a right pelvic lymphadenectomy. Pathology demonstrated a 5.9 cm high-grade urothelial carcinoma invading full thickness through the muscularis propria, pT2pN0/9R0. Approximately 15 months later she had an ipsilateral renal pelvis recurrence with lunch metastasis followed by a complete response to chemotherapy and checkpoint inhibitor therapy and refusal of consolidative surgery. She has been on surveillance and has been without disease for 2.5 years.
Moderator: Surena F. Matin, MD, MD Anderson Cancer Center, Houston, TX
Panelists: Sima Porten, MD, MPH, University of California – San Francisco, San Francisco, CA & Vitaly Margulis, MD, UT Southwestern, Dallas, TX
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the AUA2021 May Kick-off Weekend May 21-23.
References:
- Koornstra JJ, Je Mourits MJ, Sijmons RH. Management of extracolonic tumours in patients with Lynch Syndrome. Lancet Oncol. 2009;10:400-408.
- Petros FG, Qiao W, Shingla N, et al. Preoperative multiplex nomogram for prediction of high-risk nonorgan-confined upper-tract urothelial carcinoma. Urol Oncol. 2019 Apr;37(4):292.e1-292.e9.
- Freifeld Y, Ghandour R, Singla N, et al. Preoperative predictive model and nomogram for disease recurrence following radical nephroureterectomy for high grade upper tract urothelial carcinoma. Urol Oncol. 2019 Oct;37(10):758-764.


