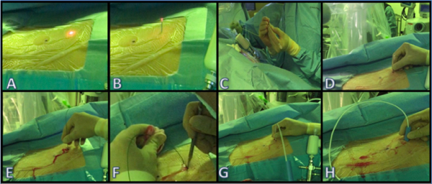
To properly select subjects, patients were screened if they had a preoperative sagittal CT tract length of < 10 cm. If consented, the patient would be pretreated with tamsulosin and ciprofloxacin for 7 days prior to surgery. In the operating room, a 16F ureteral access sheath was placed and ureteroscopic access to the kidney was established. Two cc’s of air was then injected into the ureteroscope in order to identify the air-containing, upper pole calyx with the scope. With the scope fluoroscopically confirmed in the correct position, patient respirations were suspended and the 365 µL fiber was fired with 1 J of energy at 10 Hz and was advanced towards the flank, as shown the image below. The exiting tip of the laser was grasped in the external field, then an 18-guage needle obturator was passed over the fiber into the collecting system shortly before a balloon dilator was inserted into the kidney.
In this particular study, 9 patients were consented to undergo this novel procedure. The mean operative time was 202 minutes (range: 117-250) and the mean fluoroscopic time was 32 seconds (range: 5-64). All patients were shown to have residual fragments ranging from 2.1 to 8.8 mm, however, mean absolute stone reduction was 96%. No significant ureteral injury occurred, but one Clavien grade IIIa was experienced due to a subcapsular hematoma and drop in hemoglobin. This patient was embolized and transfused with two units of red blood cells before making a full recovery.
In conclusion, Dr. Kaler described a viable new method of gaining percutaneous access with a holmium laser that may one day allow urologists to make their own accesses due to its short learning curve. Interestingly, when asked about hitting a rib by a member of the audience, Dr. Kaler explained that the laser fiber would not be able to fire if it came in contact with the bone which he claimed allows for minimal risk when exiting the kidney.
Presented by: Kam Kaler, MD
Written by: Zachary Valley, Department of Urology, University of California-Irvine, Twitter: @ZacharyAValley, at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia


