The best data for salvage radiotherapy comes from a retrospective study published more than a decade ago1. Among 1,540 patients receiving salvage radiotherapy after radical prostatectomy, the 6-year progression-free probability was 32%. Forty-eight percent (95%CI 40%-56%) of patients treated with salvage radiotherapy alone at PSA levels of 0.50 ng/mL or lower were diseases free at 6 years, including 41% (95%CI 31%-51%) who also had a PSA doubling time of 10 months or less or poorly differentiated (Gleason grade 8 to 10) cancer. In Usmani’s opinion, the keys to salvage radiotherapy are for early intervention, risk factors present for local failure (ie. positive margins), and patients at low risk for distant metastasis (ie. Gleason score ≤7).
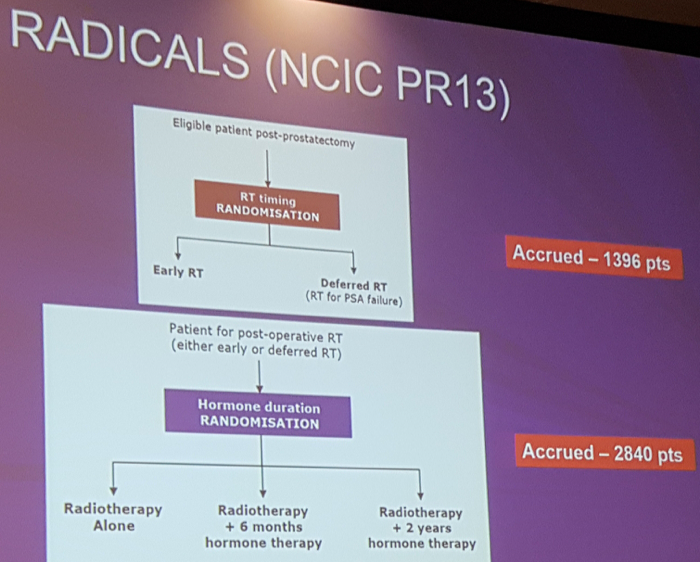
Studies comparing adjuvant vs salvage radiotherapy are historically small matched analyses, including early salvage radiotherapy (at 0.2 ng/mL) and high doses of radiotherapy used. Although fraught with selection bias, these studies suggest improved biochemical relapse-free survival with adjuvant compared to salvage radiotherapy. The RADICALS trial is a highly anticipated phase III trial comparing early to delayed radiotherapy:
Hormonal therapy is known to be beneficial in combination with radiotherapy for localized prostate cancer, acting as a radiosensitizer and to treat occult metastases. In the EORTC 22863 study, 412 high-risk prostate cancer patients were treated with either radiotherapy or radiotherapy + 3 years of ADT2. Over a median follow-up of 66 months (range 1-126), the 5-year clinical disease-free survival was 40% (95%CI 32-48) in the radiotherapy-alone group and 74% (95%CI 67-81) in the combined-treatment group (p=0.0001). The 5-year overall survival was 62% (95%CI 52-72) and 78% (95%CI 72-84), respectively (p=0.0002). In the EORTC 22961 trial, 970 high-risk prostate cancer patients were treated with radiotherapy + 6 months of ADT or radiotherapy + 3 years of ADT3. After a median follow-up of 6.4 years, 132 patients in the short-term group and 98 in the long-term group had died (47 vs 29 prostate cancer deaths). The 5-year overall mortality for short-term and long-term suppression was 19.0% and 15.2%, respectively, with a HR of 1.42 (p=0.65 for noninferiority). As such, the authors concluded that the combination of radiotherapy plus 6 months of androgen suppression provides inferior survival as compared with radiotherapy plus 3 years of ADT.
Recently, several large RCTs in the field of radiation therapy have been published. GETUG-AFU 16 assessed whether salvage radiation therapy in combination with ADT (6 months of goserelin) improves biochemical or clinical progression4. There were 743 patients randomized, and those assigned to radiotherapy plus goserelin were significantly more likely than patients in the radiotherapy alone group to be free of biochemical progression or clinical progression at 5 years (80%, 95%CI 75-84 vs 62%, 95%CI 57-67; HR 0.50, 95%CI 0.38-0.66). RTOG 9601 also assessed whether salvage radiation therapy in combination with ADT (24 months of bicalutamide) improves OS compared to salvage therapy alone5. Over a median follow-up among the surviving patients of 13 years, 760 patients were randomized. The actuarial rate of OS at 12 years was 76.3% in the bicalutamide group, as compared with 71.3% in the placebo group (HR 0.77; 95%CI 0.59-0.99). The 12-year incidence of death from prostate cancer was 5.8% in the bicalutamide group, as compared with 13.4% in the placebo group (p<0.001). The cumulative incidence of metastatic prostate cancer at 12 years was 14.5% in the bicalutamide group, as compared with 23.0% in the placebo group (P=0.005).
Usmani concluded with several take-home messages:
- There is evidence for adjuvant/salvage radiotherapy and we are awaiting the results of RADICALS for optimal timing
- There is also evidence for hormonal therapy in conjunction with salvage radiotherapy. This is an individualized decision, with patients most likely to benefit from hormonal therapy having elevated pre-RT PSAs, higher Gleason score, and nodal/seminal vesicle invasion
- A duration of 6-24 months is acceptable, with RADICALS results expected to guide optimal duration of therapy
References:
1. Stephenson AJ, Scardino PT, Kattan MW, et al. Predicting the outcome of salvage radiation therapy for recurrent prostate cancer after radical prostatectomy. J Clin Oncol 2007;25(15):2035-2041.
2. Bolla M, Collette L, Blank L, et al. Long-term results with immediate androgen suppression and external irradiation in patients with locally advanced prostate cancer (an EORTC study): A phase III randomized trial. Lancet 2002;360(9327):103-106.
3. Bolla M, de Reijke TM, Van Tienhoven G, et al. Duration of androgen suppression in the treatment of prostate cancer. N Engl J Med 2009;360(24):2516-2527.
4. Carrie C, Hasbini A, de Laroche G, et al. Salvage radiotherapy with or without short-term hormone therapy for rising prostate-specific antigen concentration after radical prostatectomy (GETUG-AFU 16): A randomized, multicentre, open-label phase 3 trial. Lancet Oncol 2016;17(6):747-756.
5. Shipley WU, Seiferheld W, Lukka HR, et al. Radiation with or without Antiandrogen Therapy in Recurrent Prostate Cancer. N Engl J Med 2017;376(5):417-428.
Presented by: Nawaid Usmani, MD, University of Alberta, Edmonton, Alberta, Canada
Written By: Zachary Klaassen, MD, Urologic Oncology Fellow, University of Toronto, Princess Margaret Cancer Centre Twitter: @zklaassen_md at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia


