PSA failure is defined as 2 consecutive PSA rises above 0.2 ng/ml. Approximately a third of the patients treated with radiotherapy experience PSA failure. The 3 possible options for management include observation, SRT (curative), and androgen deprivation therapy (ADT). SRT is highly unpredictable, and known poor prognostic factors include Gleason score 8-10, PSA > 1, PSA doubling time <10 months, and positive margins.
Imaging can be used as a response biomarker of response to SRT. It can determine recurrence location (prostate fossa vs. lymph nodes vs. distant disease). Novel tracers and imaging techniques are available today with improved accuracies. However, there are some limitations and challenges of imaging trials for SRT. These include the low sensitivity of imaging techniques used at low PSA levels (<0.5 ng/ml), interobserver variability, no comparison of imaging modalities, and the detection rates are not correlated to a strong reference standard.
Dr. Pouliot continued to describe the multicenter PROPS trial (PET/MRI pre-radiotherapy for post-prostatectomy salvage) taking place in Canada, UK, and Australia. The study design is shown in Figure 1. The primary objective was to decipher the proportion of men with negative or equivocal conventional restaging who have disease identified outside the prostate bed on other imaging modalities. Included patients were those status post radical prostatectomy with N0 or Nx, with a documented PSA rise above 0.2 ng/ml and at least one adverse feature (PSA >1 ng/ml, Gleason score >8, PSA doubling time <10 months), and all patients must have been considered for SRT.
Overall, 91 patients have been recruited, and table 1 demonstrates their characteristics. PET PSMA detected 19% of fossa recurrences and 32% of distant disease (lymph nodes and bones). The detection rates by modality are shown in Figure 2. The authors also assessed the impact of imaging on the therapeutic plan. Change in management was seen in 23% and 46% of mpMRI and FCH, respectively. The type of management was changed in 14% of cases (from curative to palliative) and in 30% (from palliative to curative).
Figure 1 – PROPS study design:
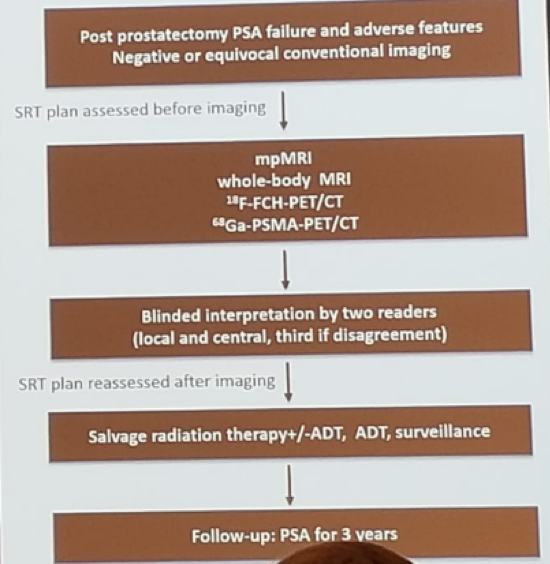
Table 1 – Patient Characteristics:
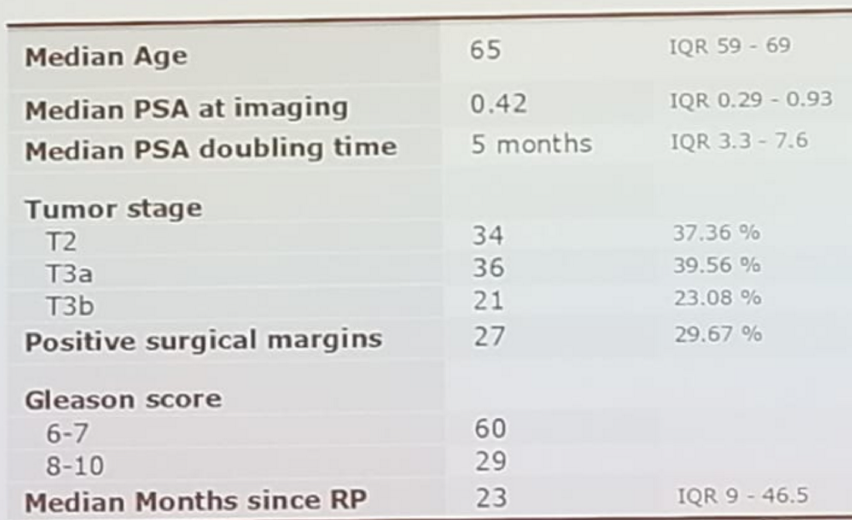
Figure 2 – Detection rates by modality:
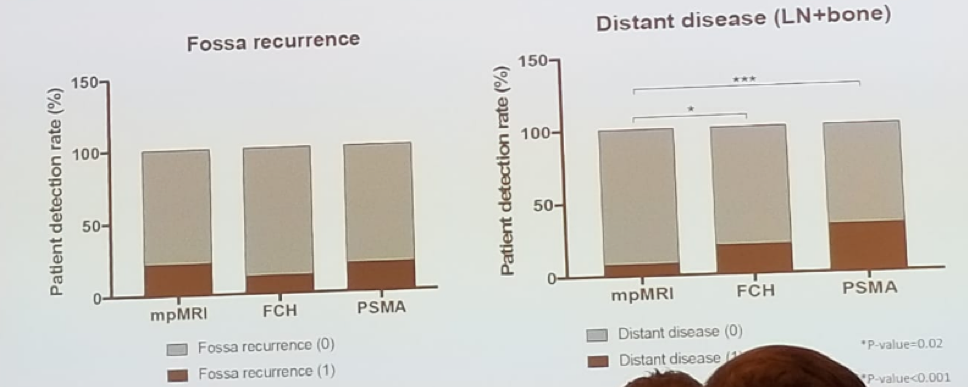
The diagnostic accuracy of metastasis detection for FCH was 47.8% and 97% sensitivity and specificity, respectively. For PET PSMA it was 66.7% sensitivity and 100% specificity.
The limitations of this study include the short follow-up time, the fact that only a subset of patients was imaged by PSMA PET/CT, and that management was not standardized, which might impact reference standard and accuracy.
Pouliot summarized his talk, stating that these molecular imaging modalities detect lesions at PSA levels for which SRT is still effective in a third of patients. It changes management in about 50% of patients, and it is highly specific and moderately sensitive when compared to reference standards. To determine if these imaging modalities add clinical benefit to current algorithms, longer follow-up is required.
Presented by: Pouliot Frederick, MD, CHU de Québec et Université Laval, Quebec, Canada
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, @GoldbergHanan at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia


