Despite effective cisplatin-based chemotherapy, the potential consequences of untreated retroperitoneal metastasis result in an inferior clinical outcome and include:
- Late relapse
- Re-operative surgery
- Somatic transformation of teratoma
To date, all the published series of late relapse demonstrate that over 85% are nonseminoma and that it occurs in the retroperitoneum in approximately 50-70% of cases. 1,2,3,4
Teratoma in the retroperitoneum increases when there was teratoma or yolk sac tumor in the primary tumor of the testis, and with increasing clinical stage and grade. The definition of somatic transformation of teratoma is components of teratoma that histologically resemble a somatic malignancy (e.g. PNET, enteric adenocarcinoma, rhabdomyosarcoma). This occurs in 0.4% of primary retroperitoneal lymph node dissection (RPLND) surgery, 3% of post-chemotherapy RPLND, 18% of redo RPLND, 21% of late relapses, and 12% of surveillance failures (with no prior chemotherapy). This occurs 6-8 times more commonly in redo RPLND than in primary RPLND, which is by itself, an independent adverse variable.
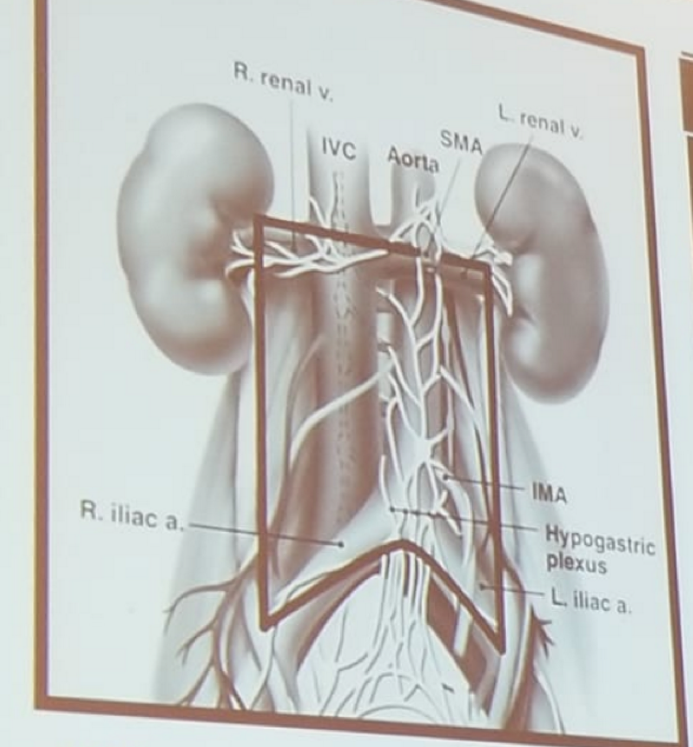
RPLND remains a critical component in the management of selected patients with GCTs. Properly performed, RPLND is both a staging and therapeutic procedure, but it should always be done with therapeutic intent. It is unclear whether this remained the case after the advent of highly effective cisplatin-based chemotherapy and improved survival rates. In the original full template bilateral RPLND (Figure 1) that was done without nerve sparing, more than 90% of patients had retrograde ejaculation.
Figure 1 – Full bilateral template:
This was the impetus for the development of modified templates (Figure 2).
Figure 2- Modified templates:
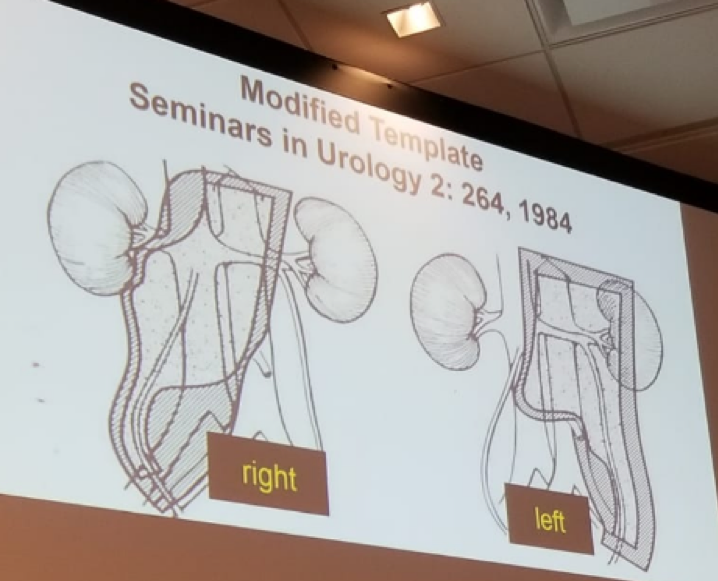
The idea behind these modified templates was to avoid dissection in areas thought to be at low (<10%) risk for disease. This risk was determined based on mapping studies (Figure 3) 5,6.
Figure 3 – Mapping studies of metastatic retroperitoneal nodes:
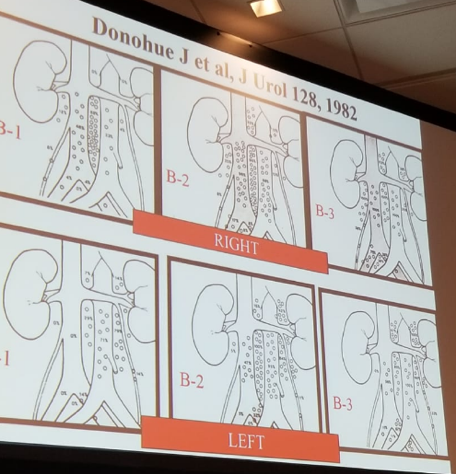
The problem with these mapping studies is that they underestimate retroperitoneal disease and cannot assess the incidence of unresected retroperitoneal disease without adequate clinical follow-up. In fact, disease outside the modified template exists in 5-38% of right modified templates, and 11-32% of left modified templates.7 Supporting the performance of full bilateral templates instead of a modified template, is the fact that the number of positive nodes resected is correlated in a linear fashion to the number of total nodes resected, and approximately 40 nodes or more are needed to be removed to make sure all positive nodes have been resected (Figure 4).8 Moreover, ipsilateral positive nodes predict contralateral positive nodes.
Figure 4 – Number of total and positive nodes removed:
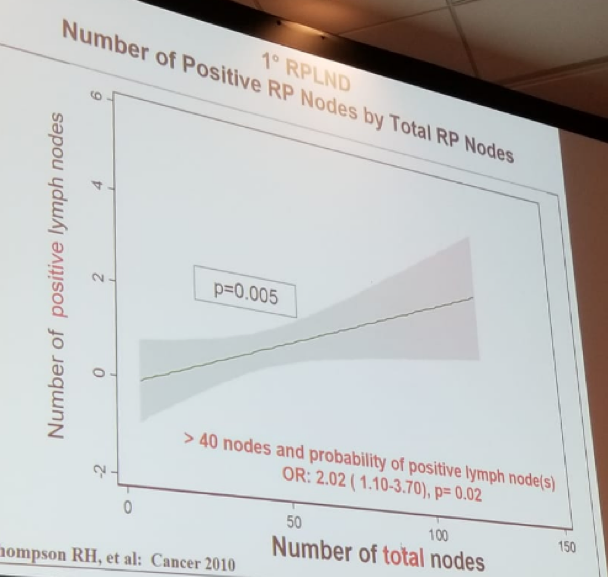
Sheinfled summarized his talk and emphasized, that due to these data, modified templates should not be performed, and a full bilateral RPLND template should always be done. In a modified template missed nodes are to be expected and extra-template metastases are not the fault of the template but a responsibility of the surgeon. Additionally, the advent of nerve-sparing techniques obviates the need for modified templates to preserve antegrade ejaculation. Bilateral template RPLND maximizes the staging and therapeutic potential of surgery. Lastly, modified templates always under-stage the retroperitoneum and unnecessarily increase the possibility of unresected retroperitoneal metastases.
References:
1. Daniel et al. JCO 1995
2. George et al. JCO 2003
3. Dieckmann et al. J Urol 2005
4. Sharp et al. JCO 2008
5. Donhaue J et al. J Urol 128, 1982
6. Weissbach L et al. J Urol 138, 1987
7. Brett S et al. JCO 2007
8. Thompson RH et al. Cancer 2010
Presented by: Joel Sheinfeld, MD, Memorial Sloan Kettering Cancer Center, New York, US
Written By: Hanan Goldberg, MD, Urologic Oncology Fellow (SUO), University of Toronto, Princess Margaret Cancer Centre, @GoldbergHanan at the 73rd Canadian Urological Association Annual Meeting - June 23 - 26, 2018 - Halifax, Nova Scotia


