The authors of this study, in an effort to address this, compare pathologic characteristics of patients who underwent RP after initiating AS, and then compared them to patients eligible for AS but who chose to undergo immediate RP. Additionally, they note that no prior study had looked at tumor volume (TV) in the pathologic specimen.
Between 2009 and 2016, they enrolled 235 consecutive patients into their AS program for low-risk PCa according to the PRIAS criteria (cT1/T2a; PSA<10 ng/ml; PSA density <0.2; Gleason score <7; < 3 positive cores). 88/235 patients (37.4%) were ultimately treated with active therapy for rising PSA, pathological upgrading (Gleason>6 or >2 positive cores) or patient preference. Of these, 48 patients (55%) were submitted to RP - median time from AS entry to RP was 14 months (IQR: 11-25.5). Amongst other pathologic variables, TV (mL) was calculated as prostate weight x percentage of cancer at whole mount pathology. The comparison cohort was 274 AS-eligible men who underwent immediate RP.
Below is a summary of the findings between the two groups.
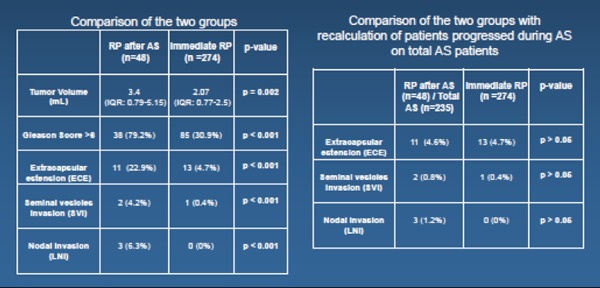
When the two groups were compared (left table), patients initially managed with AS had higher rates of Gleason > 6 (7.7% vs. 35.4%), ECE (22.9 vs. 4.7%), SVI (4.2 vs. 0.4%), LNI (6.3 vs. 0%) and higher (all p<0.001). However, when the rates of adverse pathology of patients who progressed during AS (n=48) were recalculated on the total number of patients who entered the AS program (n=235) (right table), these figures were virtually identical to those of patients submitted to immediate RP (ECE: 4.6 vs. 4.7%; SVI: 0.8 vs. 0.4%; LNI: 1.2 vs. 0%, all p = NS), suggesting that time on AS did not worsen pathological outcomes.
The correction for the original AS cohort is a nice addition to the study. Otherwise, the self-selected group will always look worse than the immediate RP group.
I agree with the authors when they conclude the following: The findings of adverse pathology at RP seem to be more related to initial misclassification instead of real clinical progression.
Limitations / Discussion Points:
The moderators made a point to note that the 14 months to intervention seemed fast, which is concerning for a poorly selected population.
This relates to a point made during this group’s poster yesterday (see our summary for “First repeated biopsy represents the most informative predictor of progression-free survival at 3 years follow-up in patients included in an active surveillance protocol for low-risk prostate cancer”) where this group does not routinely do AS confirmatory biopsy.
Speaker(s): S. Lugazzo
Co-Authors: Suardi N., Dell'Oglio P., Fossati N., Gandaglia G., Zaffuto E., Gaboardi F., Doglioni C., Freschi M., Scattoni V., Stabile A., Montorsi F., Briganti A.
Written By: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto
Twitter: @tchandra_uromd
at the #EAU17 - March 24-28, 2017- London, England


