In this study, the authors at UCL (London), who have a long-history with the use of mpMRI, highlight the findings of their mpMRI-based active surveillance regimen. This is a single-center experience.
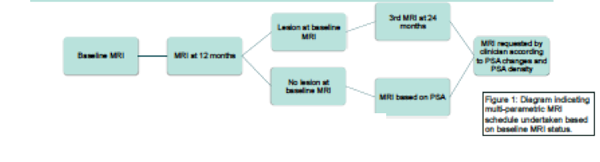
In their AS regimen, the utilize mpMRI heavily. Below, they highlight the stratification process for follow-up MRI’s – based on the presence or absence of a lesion on the initial MRI’s.
Limitations / Discussion Points:
The inclusion criteria were men who met the NICE guidelines for active surveillance (Gleason
score 3+3 or 3+4, PSA< 20ng/ml) and had an mpMRI at UCLH. Biopsies (MRI-targeted, transperineal) were performed for the following reasons: a lesion was discordant with the
original histology, progression on mpMRI, or according to a change in other factors (eg an
increase in PSA density). It should be noted that even without a lesion on baseline MRI, all men usually received another MRI every 3 years.
A recommendation for active treatment was discussed based on mpMRI features and in those men who showed other high risk features (Gleason 8 disease, or any nodal or metastatic disease).
Of this AS cohort, 387 men met inclusion criteria and were initiated on AS between 2004 and 2015. Of the 387, 64 (17%) had Gleason 3+4 prostate cancer. By the time of analysis, 294 men remained on AS (median time 5 years); 64 men went on to active treatment.
No prostate cancer related death occurred in the cohort. The 5-year treatment free survival was 85.1% and 78.3% for men without and with lesions on baseline mpMRI, respectively (p=0.024). The 5-year treatment free survival was 86.3% and 60.8% in patients with Gleason 3+3 and 3+4, respectively (p<0.001).
Ultimately, the authors conclude that a lesion on mpMRI and Gleason 3+4 disease predict worse outcomes. However, the Gleason 3+4 finding is not unsurprising, and many institutions would not consider them for AS. It would have been cleaner for the authors to only consider the Gleason 6 patients. More detail regarding their MRI findings (besides just lesion presence/absence) would be helpful guide future management – per the presenter, they are looking into this now.
Regardless, the use of mpMRI will likely be an important part of many institutions’ AS protocols.
Speaker(s): Adam Retter
Co-Authors: Giganti F., Kirkham A., Allen C., Punwani S., Emberton M., Moore C.
Institution(s):
1. University College London Hospital, Dept. of Radiology, London, United Kingdom
2. University College London Hospital, Dept. of Urology, London, United Kingdom
Written By: Thenappan Chandrasekar, MD, Clinical Fellow, University of Toronto
Twitter: @tchandra_uromd
at the #EAU17 - March 24-28, 2017- London, England


