MRI targeted fusion biopsy showed GGG3 disease in 2/3 cores from the region of interest as well as GGG2 in 4 of 12 systemic cores. Staging investigations were negative so he proceeded to local therapy, opting for radical prostatectomy. He underwent RALP and extended pelvic lymphadenectomy with final pathology showing pT3a pN0 (0/16) Gleason score 4+3 (GGG3) prostate cancer with negative margins. His initial post-operative PSA was undetectable but approximately 1 year following surgery, he presented with a rising PSA. This was observed over the course of 6 months where it rose to 0.4 ng/mL and he underwent salvage radiotherapy to the prostate bed and pelvis, along with 6 months of concurrent androgen deprivation therapy. His PSA then became undetectable again but rose again just over 1 year following salvage radiotherapy.
To investigate this rising PSA, a prostate-specific membrane antigen (PSMA) PET/CT was performed when his PSA was 0.7 ng/mL. As shown here, this showed no evidence of local recurrence and no bony lesions but a small, suspicious lymph node in the perirectal fat.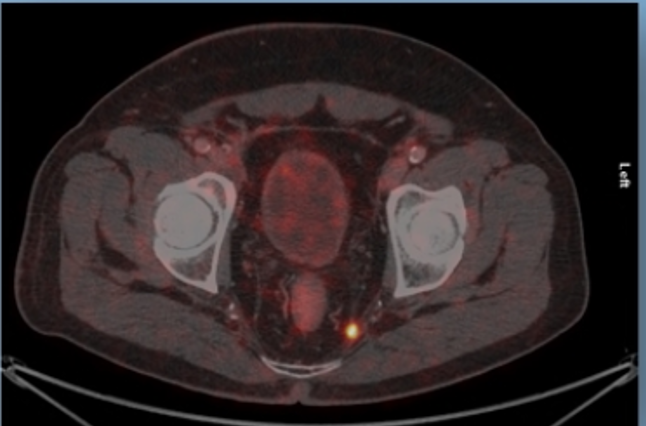
This was treated with a 35 Gy SBRT boost, without concurrent androgen deprivation. PSA then remained low, but detectable (0.1 ng/mL).
This case set the stage for subsequent presentations assessing the role of imaging first or treatment first in patients with biochemically recurrent disease.
Presented by: Annika Herlemann, MD, Ludwig-Maximilians-University of Munich, Munich, Germany
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, Twitter: @WallisCJD at the 35th Annual EAU Congress, 2020 Virtual Program #EAU20, July 17-19, 2020.


