Dr. Hadaschik began by highlighting older data from MSKCC demonstrating that Gleason score (i.e. tumor grade as a proxy for biology) is the most important predictor of long-term outcomes for patients with localized prostate cancer undergoing local therapy.
He then highlighted data from the PROMIS study demonstrating that TRUS biopsy has relatively poor sensitivity for clinically significant disease while MRI guided biopsy has a 93% sensitivity, compared to template mapping biopsy.
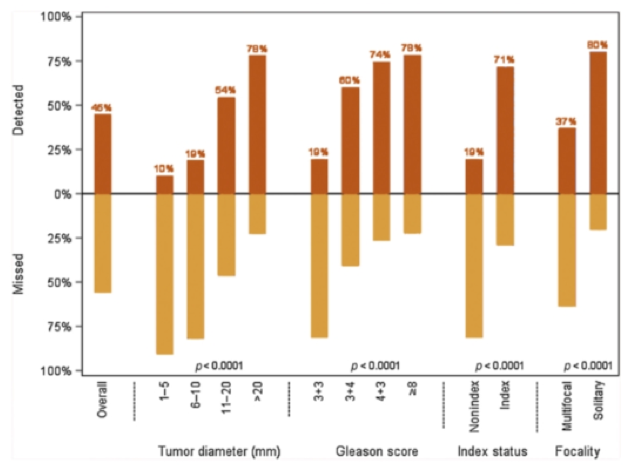
However, he acknowledged that there are limitations to prostate MRI including under-detection of non-index tumors and smaller lesions. However, miss rates are highest among tumors least likely to be clinically significant.
Beyond limitations in the MRI itself, there are limitations in MRI-guided fusion biopsy in part due to random error introduced in the fusion and registration process. Updated data from the NIH which he cited demonstrates a small but non-zero miss rate when a systematic biopsy is omitted (5.8% of GG2 or greater and 1.9$ of GG3 or greater disease).
He then cited data clearly demonstrating that the addition of MRI based information to a clinical dataset improves risk modeling, with significantly improved risk model AUCs. This is also valuable in staging, with a risk model integrating MRI improves predicting of extraprostatic extension at the time of radical prostatectomy and predicting lymph node invasion at the time of radical prostatectomy. In an update of the Briganti nomogram published in 2019, grade group of MRI-targeted biopsy is very influential in the risk of lymph node involvement. While systematic biopsy results remain influential, it is the percentage of positive cores that are now included in the model.
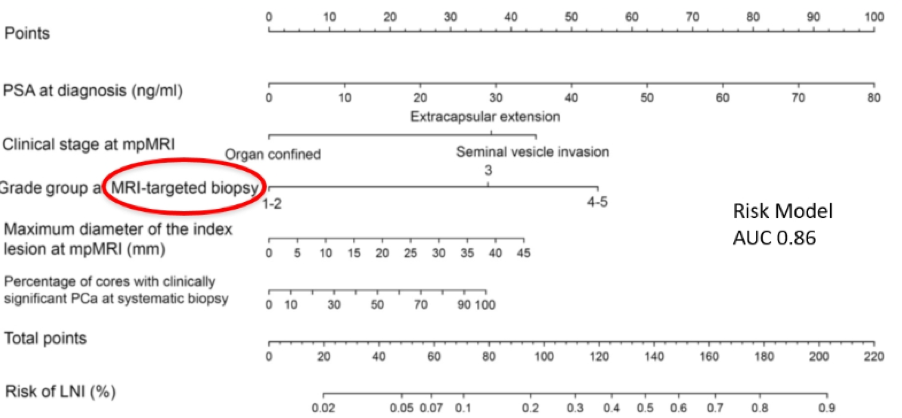
It is important to highlight that the NUMBER of positive targeted cores is not an important predictor of clinical outcomes as this depends more on operator technique than underlying biology.
The use of the novel nomogram increases the ability to spare lymphadenectomy.
He then moved to an assessment of correlates between genomic and imaging findings, demonstrating that these often correlate but that there is unlikely to be large value for risk prediction in the absence of a visualized index lesion.
He then moved to a discussion of PSMA PET/CT. Presented at this year’s EAU was the proPSMA trial which demonstrated the value of this approach in initial staging prior to local therapy. He then wondered whether the value of nomograms would be retained with more accurate imaging. However, recent data from OSPREY demonstrated that even PSMA misses lymph node metastases.
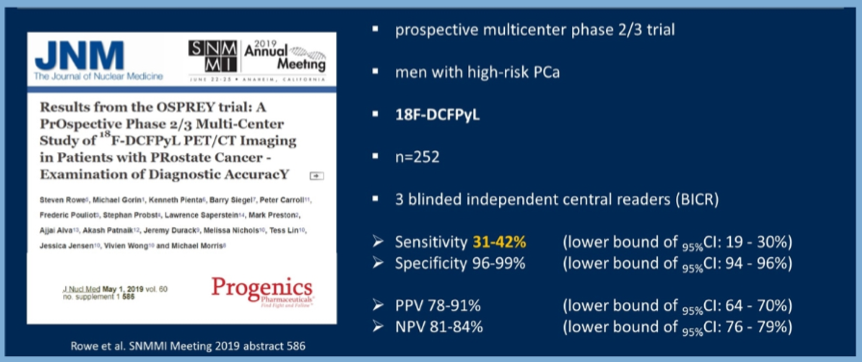
Thus, even with more sensitive imaging approaches, there likely remains a role for prognostic nomograms to inform care.
Presented by: Boris A. Hadaschik, MD, Chairman, Department of Urology, University Hospital Essen
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center Contact: @WallisCJD on Twitter at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020


