(UroToday.com) The focal therapy for prostate cancer thematic session at the virtual European Association of Urology (EAU) 2020 Annual Meeting featured two talks on the outcome of salvage radical prostatectomy after focal therapy, with Prasanna Sooriakumaran, MBBS, discussing the poor ability to achieve good function and pathological results after this procedure.
The traditional experience with salvage prostatectomy is such that <5% of patients with biochemical recurrence after radiotherapy/focal therapy receive salvage radical prostatectomy. This is secondary to concerns for difficult planes, tough tissues, an insecure anastomosis, and poor functional outcomes. Furthermore, most of the early experience was with open salvage radical prostatectomy after primary radiotherapy. However, there have been several changes over the past decade, including the advent of salvage robotic radical prostatectomy after radiotherapy, which has allowed better vision, a better anastomosis, and better outcomes, as well as salvage robotic prostatectomy after focal therapy. Intuitively, ‘focal’ primary therapy may have less impact when it comes to salvage therapy. There is limited available evidence for salvage robotic prostatectomy after focal therapy and our knowledge about its indications and outcomes is still evolving.
At the University College London Hospital between 2011 and 2019, there were 126 patients that underwent a salvage robotic prostatectomy, including 46 men after radiotherapy and 80 men after focal therapy. The type of primary focal therapy included 72 patients undergoing HIFU, 4 undergoing cryoablation, 3 undergoing electroporation, and one patient undergoing radiofrequency ablation. The breakdown for the template of primary focal therapy is as follows: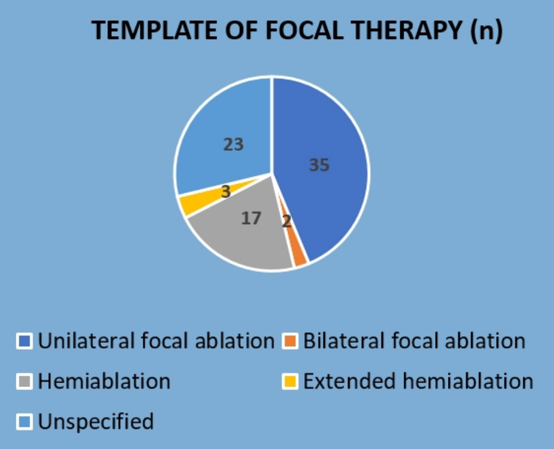
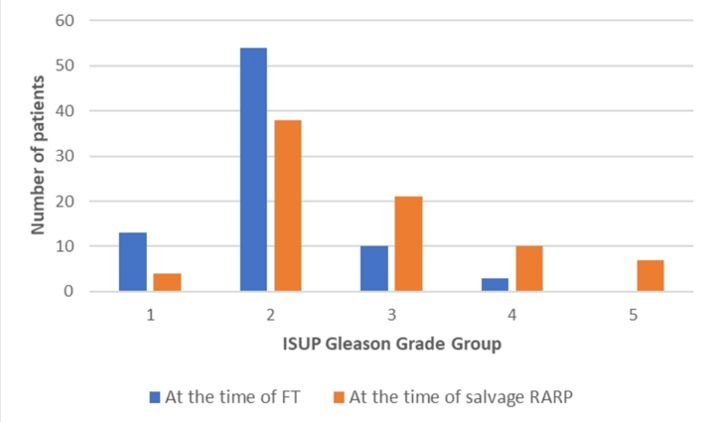
Among the patients undergoing salvage robotic prostatectomy after primary focal therapy, the median age was 67 years (IQR 61-69) and the median PSA was 5.5 ng/mL (IQR 3.5-10). 26.2% of patients had GG3 disease, 12.5% GG4, and 8.7% GG5 prostate cancer. This corresponded to a Gleason upgrading rate from focal therapy to the time of salvage robotic prostatectomy of 46.2%; time to salvage robotic prostatectomy was 29 months (IQR 19-52). The mean operating time was 160 min, mean blood loss was 200 mL, and there was only case of a rectal injury, thus demonstrating that salvage robotic prostatectomy after focal therapy is safe and feasible. Additionally, the Grade 1-2 complication rate was 10% and 6.2% for Grade >=3, demonstrating that salvage robotic prostatectomy has an acceptable complication rate after primary focal therapy. The following graph demonstrates the Gleason Group upgrading at the time of salvage robotic prostatectomy:
In terms of additional oncological outcomes, over a median follow-up of 19 months (IQR 10-30), 69% of patients had no recurrence, 8.75% of patients had PSA persistence, and 22.5% of patients had a biochemical recurrence. The margin status at the time of salvage radical prostatectomy is as follows:
At three months, 35% of patients were fully continent, which increased to 68.7% at six months post-operatively. At the other end of the spectrum, 27.5% of patients were severely incontinent (>= 3 pads/day) at three months, whereas this improved to 10% at six months. 63% of salvage robotic prostatectomies were non-nerve sparing, 32.5% were unilateral, and 5% were bilateral nerve-sparing. At three months postoperatively, 92.5% of patients reported erectile dysfunction.
Dr. Sooriakumaran concluded his presentation with the following take-home messages:
- Salvage robotic radical prostatectomy is feasible and safe
- Almost half the patients who receive focal therapy get upgraded by the time they require salvage surgery
- Many patients belong to the high-risk category at the time of salvage robotic prostatectomy
- Salvage robotic prostatectomy was associated with poor pathological (worse disease after focal therapy), functional (erectile dysfunction) and oncologic (biochemical recurrence) outcomes compared to primary robotic prostatectomy
- Focal therapy can be an attractive option for patients, but when it fails, patients will usually be worse off than if they opted for primary robotic prostatectomy
- It is important to get the first treatment right so as to try and avoid the need for salvage robotic prostatectomy
Presented by: Prasanna Sooriakumaran, MBBS, PhD, University College London Hospital, London, UK
Written By: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, GA, USA, Twitter: @zklaassen_md, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.


