(UroToday.com) Dr. Loidl gave a talk about the use of imaging in castrate-resistant prostate cancer (CRPC). According to Dr. Loidl, an important question to ask is when and what type of imaging is appropriate and in which scenario of prostate cancer.
The advanced prostate cancer consensus conference 2017 guideline recommended that imaging be performed at baseline, PSA nadir, and progression, at least in patients with the usual presentation of metastatic hormone-sensitive prostate cancer, and castrate-resistant prostate cancer.
As recommended by the prostate cancer working group 3 consensus statements, PSA progression alone for men on the treatment of metastatic CRPC should not be the sole reason to change therapy.
Based on the growing knowledge, a new endpoint for clinical studies in CRPC was created - the radiographic progression-free survival (rPFS). Recently, a new era had begun with the approval of more than eight drugs in the treatment of castrate-resistant prostate cancer, based on positive studies, including radiographic progression-free survival as an endpoint.
Conventional imaging has included CT scans, bone scan, and MRI. The next-generation imaging includes Ga-PSMA, F-fluciclovine PET CT/MRI, and whole-body MRI.
CT scan has several limitations, including a relatively poor performance for the detection of bone metastasis and limited assessment of lymph node metastasis.
MRI’s limitations include longer examination times and the fact that the detection of lymph node metastasis is done with the same morphological features that are assessed with CT scans. The sensitivity and specificities of CT are 42% and 82%, respectively, while the sensitivity and specificity of MRI are 39% and 82%, respectively.
Bone scan also has limitations, which include the fact that new bone formations responding to therapy can appear as a new lesion, which is called the ‘flare response.’ Therefore, the prostate cancer working Group 3 guidelines require new bone lesions to be seen on two consecutive scans, and new lesions to be seen on the second scan before progression can be defined. Other limitations include an inherent delay to the need for confirmatory scans and difficulties in quantifying disease and therefore track progression.
PSMA-PET CT for early castration-resistant prostate cancer was shown to be positive in 75% of patients with 29% of patients having local disease only and 45% of the patients having metastatic disease.
According to the European Association of Urology (EAU) guidelines, choline PET/CT, PSMA PET/CT, and MRI provide a more sensitive detection rate of lymph nodes and bone metastasis than the classical work up associated with bone scans and abdominopelvic CT scan. Although it might be tempting to conclude that bone scans and CT scans should be replaced by more sensitive tests in all patients undergoing initial prostate cancer staging, the clinical benefit of detecting metastasis at an earlier time point remains unclear!
The prognosis and ideal management of patients diagnosed as metastatic by these more sensitive imaging tests are currently unknown. It is still unclear whether patients with metastasis, detectable only with PET CT or MRI, should be managed using systemic therapies or whether they should be submitted to aggressive local and metastasis directed therapies.
Data from SPARTAN1, PROSPER2, and ARAMIS3 trials show that the treatment of high-risk non-metastatic castrate-resistant prostate cancer patients with systemic therapies added two ongoing ADT can delay the transition to metastatic castrate-resistant prostate cancer. Therefore, metastatic disease on PSMA-PET should not disqualify patients from receiving treatment with androgen receptor inhibitors.
Despite its many advantages, there are certain limitations in the use of PET-CT/MRI. It has been shown that the expression of mPSMA and diagnosis was associated with higher Gleason grade and worse overall survival. mPSMA expression levels increased at metastatic castrate-resistant prostate cancer compared to hormone-sensitive prostate cancer (55 vs. 17.5). Surprisingly, 42% of hormone-sensitive prostate cancer and 27% of metastatic castrate-resistant prostate cancer tissues have shown no detectable mPSMA.
Lastly, marked intratumor heterogeneity of mPSMA expression, with foci containing no detectable PSMA, was observed in all mPSMA expressing hormone-sensitive prostate cancer and 84% of metastatic castrate-resistant prostate cancer biopsies. These and other data prove that clinicians cannot solely rely on PSMA in metastatic castrate-resistant prostate cancer patients.
Dr. Loidl moved on to discuss when additional imaging is needed in castrate-resistant prostate cancer patients:
- Exclusively visceral metastasis
- Radiographically predominant lytic bone metastases by plain X-Ray or CT scan
- Bulky (>=5 cm) lymphadenopathy or bulky (>=5 cm) high-grade (>=Gleason 8) tumor mass in the prostate or pelvis
- Low PSA (<=10 ng/ml) at initial presentation plus high-volume (>=20) bone metastases
- Presence of neuroendocrine markers on histology or in serum
- Raised carcinoembryonic antigen
- Short interval (<=6 months) to androgen-independent progression following the initiation of hormonal therapy
Dr. Loidl concluded his talk emphasizing that new generation imaging can be offered only if a change in clinical care is contemplated. Assuming patients have received or are ineligible for local salvage treatment options, new generation imaging may clarify the presence or absence of metastatic disease, but the data on detection capabilities of new generation imaging in this setting, and the impact on management are still limited. Importantly, in patients with metastatic castrate-resistant prostate cancer with clear evidence of radiographic progression on conventional imaging while new generation imaging should not be routinely offered. New generation imaging could play a role if they are performed at baseline to facilitate comparison of imaging findings or extent of disease progression.
Dr. Loidl ended his discussion with some important take-home messages. These include the concept that there is clearly a value in PET-PSMA imaging. However, many times there is no significant added value in this imaging to the management plan that has already been decided upon. There are many situations where PET PSMA imaging will not alter the decided treatment plan, and therefore it is not worth performing.
There are many upcoming studies in the near future that will help us answer some pressing questions regarding new generation imaging studies, with various forms of PET scans, including immune-PET with PD-1/PD-L1 (Table 1).
Other compounds that will be assessed with novel imaging include CD8+ T cells antibody fragments, and Granzyme B (a serine protease released from CD8+ T cells and natural killer cells).
Table 1 – Ongoing and awaited clinical PD-1/PD-L1 imaging studies: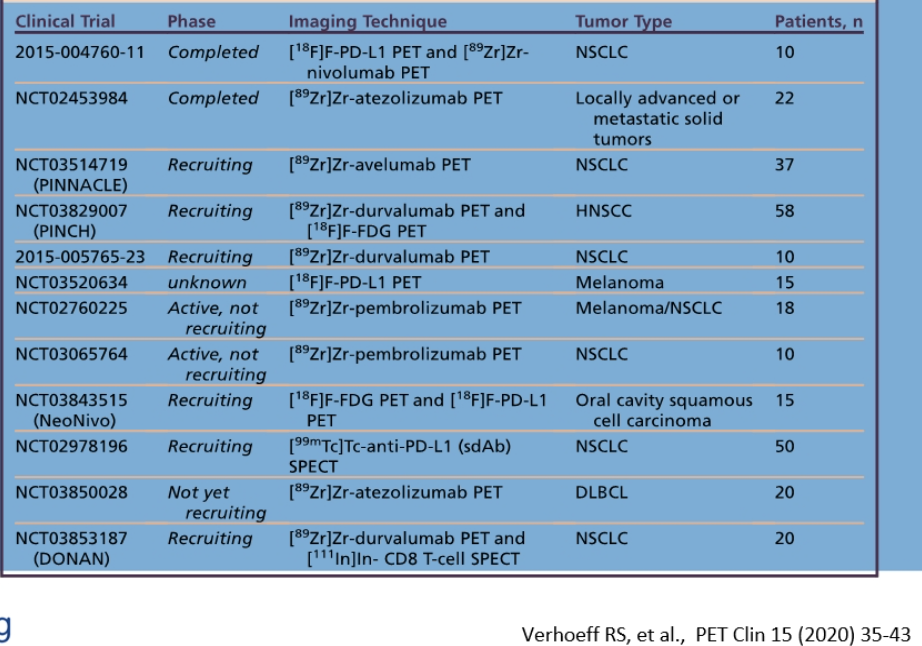
Presented by: Wolfgang Loidl, MD, Ordensklinikum Linz, Austria
Written by: Hanan Goldberg, MD, MSc., Urology Department, SUNY Upstate Medical University, Syracuse, NY, USA @GoldbergHanan at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
References:
- Smith MR, Saad F, Chowdhury S, et al. Apalutamide Treatment and Metastasis-free Survival in Prostate Cancer. New England Journal of Medicine 2018; 378(15): 1408-18.
- Hussain M, Fizazi K, Saad F, et al. Enzalutamide in Men with Nonmetastatic, Castration-Resistant Prostate Cancer. New England Journal of Medicine 2018; 378(26): 2465-74.
- Fizazi K, Shore N, Tammela TL, et al. Darolutamide in Nonmetastatic, Castration-Resistant Prostate Cancer. New England Journal of Medicine 2019; 380(13): 1235-46.


