(UroToday.com) Prostate membrane antigen (PSMA) is a type 2 transmembrane protein with an enzymatic function of a folate hydrolase carboxypeptidase. It is expressed in several tissues with different functions, including activity in Glial cells, modulating signal transduction pathway, in the small intestine, assisting in fulling absorption, and it has an uncertain role in the prostate (figure 1).
Figure 1 – The various roles of PSMA:
PSMA has significant clinical utility in prostate cancer, demonstrating detection rates for bone metastasis of 93.9% when PSA values are over two ng/ml in metastatic castration-resistant prostate cancer (mCRPC). However, not all patients respond to PSMA targeting drugs, and there's even significant inter- and intra- patients' heterogeneity (Figure 2).
Figure 2 – PSMA heterogeneity:

The hypothesis is that PSMA facilitates folate transport in prostate cancer cells. Its overexpression could represent an adaptive response to the increased requirement of folate. Prostate cancer cells with DNA damage repair aberrations have increased DNA synthesis and repair. Therefore, they need higher levels of PSMA to acquire folates so that they could increase the nucleotide pool.
Although not all patients express Membranous PSMA (mPSMA), the ones that do show higher levels of mPSMA expression were shown to be associated with having a higher Gleason grade and worse overall survival, demonstrating that PSMA has a prognostic role as well (Figure 3).
Figure 3 – Prognostic role of PSMA expression1:

When assessing the conversion of hormone-sensitive PCa to CRPC, mPSMA expression increased in matched samples (figure 4). mPSMA expression has been associated with deleterious DNR repair aberrations.
Figure 4 – mPSMA protein expression from hormone-sensitive to CRPC – matched samples: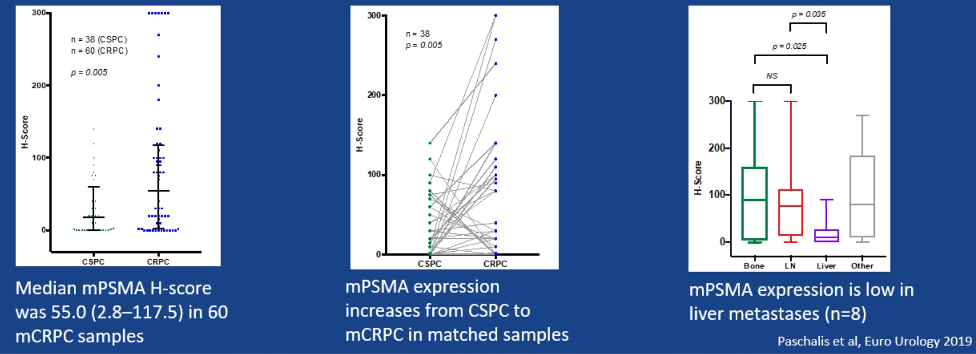
Although the presented data is retrospective and with relatively small sample size, these data do suggest that PSMA expression in mCRPC presents a degree of inter- and intrapatient heterogeneity. Tumors with DNA damage repair mutations might be more likely to benefit from PSMA targeting agents. Lastly, PSMA expression could reflect a "stressed" phenotype requiring a higher pool of folate. Naturally, these data would need to be further evaluated in prospective and larger trials.
Presented by: Pasquale Rescigno, MD, Clinical Research Fellow at The Institute of Cancer Research, London, United Kingdom
Written by: Hanan Goldberg, MD, MSc., Urology Department, SUNY Upstate Medical University, Syracuse, NY, USA, @GoldbergHanan at the 35th Annual EAU Congress, 2020 Virtual Program #EAU20, July 17-19, 2020.


