First assessing the question of a man with a negative MRI, Dr. Lamb considered the question of the negative predictive value of MRI. It’s important to consider that there are two definitions of MRI (PIRADS < 3 and PIRADS <4) as well as two definitions of clinically significant prostate cancer (GGG 2-5 and GGG 3-5). He cited a systemic review of 42 studies published between 2016 and 2020 reporting on 7321 men. Overall, these data demonstrated a negative predictive value of 91%, as Dr. Ahmed also discussed in his presentation on MRI as a triage test.
Patients (and physicians) may wonder if it is reasonable and safe to forgo biopsy in men with a negative MRI. Dr. Lamb suggested that it was, except for men with elevated PSA density. He suggested that biopsy would still be usually indicated for patients with PSAD > 0.15 ng/mL, though thresholds of 0.1 or 0.2 ng/mL would also be considered. Citing evidence published by Venderink and colleagues, 42% of patients with a PIRADS lesion could avoid biopsy if using a threshold of PSAD >0.15ng/mL with only 6% (95% confidence interval 2-15%) of clinically significant cancers being missed. Dr. Lamb also highlighted other reasons that may prompt biopsy in the setting of a negative MRI including patient concern and doubt of the MRI (for reasons including hip prostheses, very large prostates, and young patients).
When opting not to biopsy in the setting of a normal MRI, Dr. Lamb highlighted two philosophical approaches ranging from “close monitoring” to a non-interventional approach.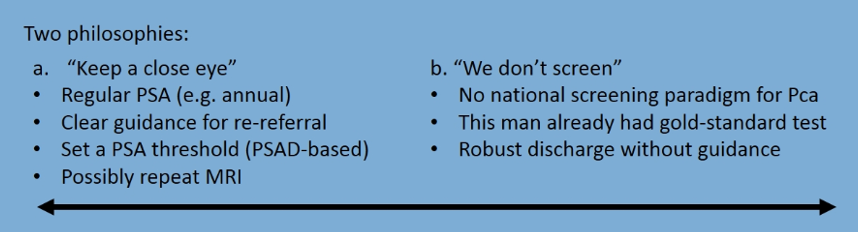
Dr. Lamb closed this question by suggesting that patient-centered decision making should form the basis of our approach to patients with a negative MRI. We need to be transparent about the false-negative rates and be open to the idea of biopsy in this setting, particularly when considering PSA density, patient concern, and specific MRI technical shortcomings.
Dr. Lamb then transitioned to assessing the question of how to manage patients who had a negative biopsy. As with how he concluded the discussion of the patient with a negative MRI, he began this discussion highlighting the EAU-EANM-ESTRO-ESUR-SIOG guidelines on prostate cancer.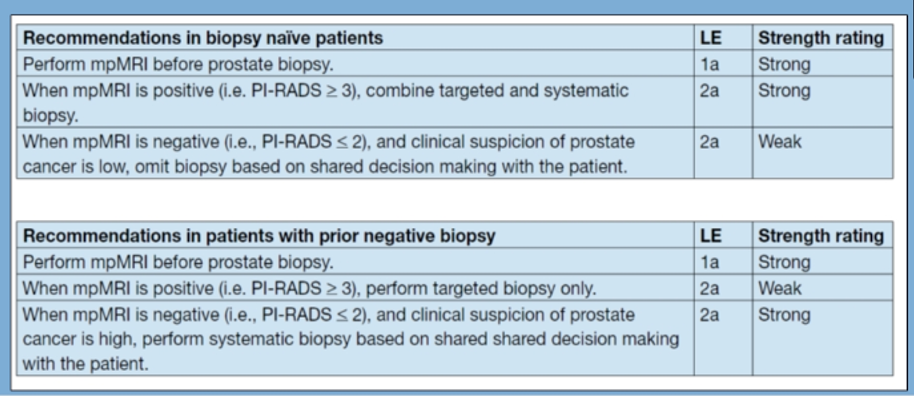
As with the initial discussion of initial negative MRI, we must consider the negative predictive value in this context. Again highlighting data from a recent systemic review, the negative predictive value in this clinical context (with a prior negative biopsy) is 93% based on pooled data, even higher than in the upfront setting.
In patients who have had a prior negative TRUS biopsy, Dr. Lamb highlighted outcomes of local anesthetic transperineal biopsy demonstrating 34% chance of clinically significant prostate cancer in those with PIRADS 4 and 5, 49% chance in those with an anterior MRI lesion, and 33% chance in those with apical lesion on biopsy.
Short of another biopsy, Dr. Lamb highlighted numerous other tests that may be useful for risk stratification. A number of these are described in the EAU-EANM-ESTRO-ESUR-SIOG guidelines.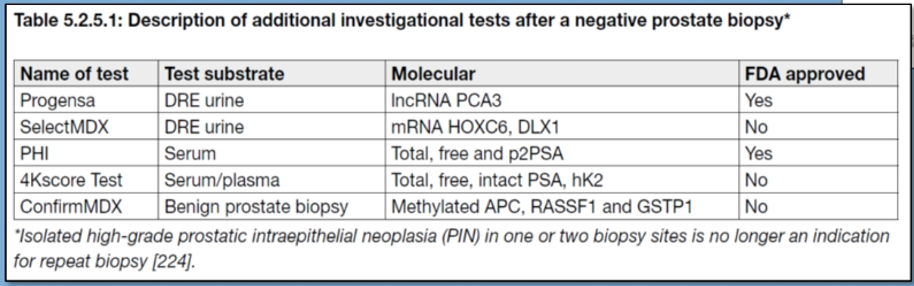
Again, we can consider two philosophical approaches here, one more aggressive (keeping a “close eye”) and one more conservative, on the basis of patient characteristics and concerns, as well as clinical characteristics.
Presented by: Alastair Lamb Ph.D, FRCS(Urol), Nuffield Department of Surgical Sciences, University of Oxford
Written by: Christopher J.D. Wallis, Urologic Oncology Fellow, Vanderbilt University Medical Center, @WallisCJD on Twitter at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.


