(UroToday.com) As part of the thematic session on salvage lymph node dissection for prostate cancer at the annual European Association of Urology 2020 virtual meeting, Alberto Briganti, MD, from Milan, Italy discussed the role of early diagnosis in these patients. Dr. Briganti started by noting that whether early detection of nodal metastasis is helpful to the patient is still (almost) unknown in 2020.
First, primary staging is important for these patients. In a review of the current literature assessing the role of 68Ga-PSMA PET for detecting lymph node metastases,1 nine retrospective and two prospective studies described the sensitivity and specificity of 68Ga-PSMA PET for detecting pelvic lymph node metastases before initial treatment, which ranged from 33.3% to 100% and 80% to 100%, respectively. Furthermore, the detection rate of 68Ga-PSMA PET in patients with biochemical recurrence after radical prostatectomy in the prostate-specific antigen (PSA) subgroups <0.2 ng/mL, 0.2-0.49 ng/mL and 0.5 to <1.0 ng/mL ranged from 11.3% to 50.0%, 20.0% to 72.7% and 25.0% to 87.5%, respectively. These results are summarized in the following table: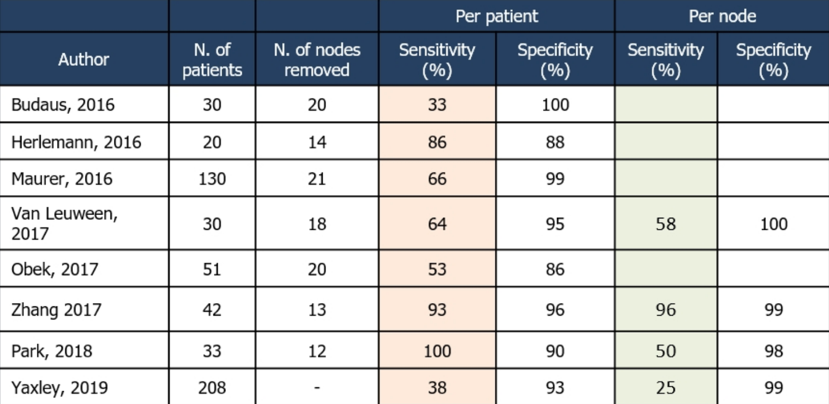
The much-heralded proPSMA study was also recently published in The Lancet assessing PSMA PET in patients with high-risk prostate cancer before either radical prostatectomy or radiotherapy.2 Among 302 men eligible, 152 (50%) were randomly assigned to conventional imaging and 150 (50%) to PSMA PET-CT. Of 295 (98%) men with follow-up, 87 (30%) had pelvic nodal or distant metastatic disease, and PSMA PET-CT had a 27% (95% CI 23-31) greater accuracy than that of conventional imaging (92% [95% CI 88-95] versus 65% [95% CI 60-69]; p<0·0001) for detecting nodal disease. Additionally, there was a lower sensitivity (38% [95% CI 24-52] versus 85% [95% CI 74-96]) and specificity (91% [95% CI 85-97] versus 98% [95% CI 95-100]) for conventional imaging compared with PSMA PET-CT. In addition to improved nodal detection with PSMA PET, these findings also altered management for patients: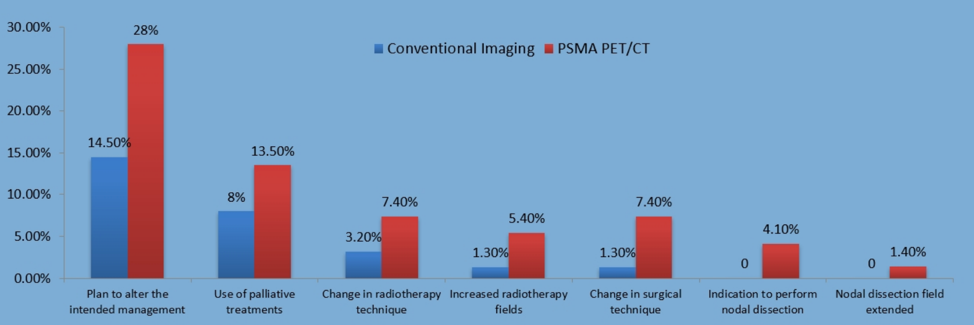
However, as Dr. Briganti notes, it is unknown whether this change in primary management is associated with improved patient oncological outcomes. Evidence on the efficacy of systemic treatment is hormone-sensitive prostate cancer is still based on conventional imaging only. Furthermore, studies evaluating the role of local therapies in oligometastatic patients are also based on conventional imaging only.
The impact of early detection of biochemical recurrence also has imaging ramifications. As follows is a summary table of the performance characteristics of prostate-specific membrane antigen (PSMA) positron emission typography (PET)/computed tomography (CT) in the biochemical recurrent disease space: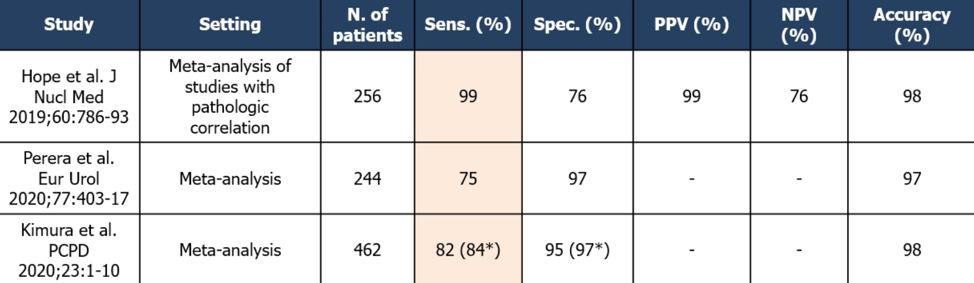
However, it is important to note that PET/CT underestimates the real nodal burden of disease. In recently published work from Dr. Briganti’s group [3], among 641 patients who experienced PSA rise and nodal recurrence after radical prostatectomy who underwent salvage lymph node dissection, lymph node recurrence was documented by PET/CT using 11C-choline (407, 63%) or 68Ga-PSMA ligand (234, 37%). The extent of tumor burden underestimation was significantly higher in the 11C-choline group compared to the 68Ga-PSMA group (p <0.0001). Furthermore, tumor burden underestimation was lower with 68Ga-PSMA only when PSA was <= 1.5 ng/ml.
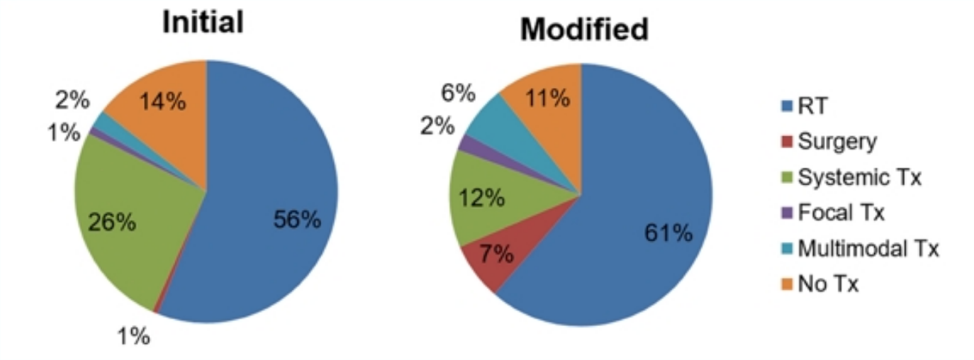
Ultimately, the question is if PSMA PET/CT imaging changes management at the time of biochemical recurrence. In a systematic review by Han et al.4 assessing the impact of PSMA PET on changes to management, the pooled proportion of management changes was 54%. Furthermore, the proportion of radiotherapy (from 56% to 61%), surgery (from 1% to 7%), focal therapy (from 1% to 2%), and multimodal treatment (from 2% to 6%) increased. Interestingly, the proportion of systemic treatment (from 26% to 12%) and no treatment (from 14% to 11%) decreased.
As Dr. Briganti notes, it is (still) unknown if these changes in the management of recurrence is associated with improved patient oncological outcomes, but data is growing. As follows is a table summarizing the implications of a positive PSMA PET/CT scan from randomized phase II trials, including "Surveillance or Metastasis-Directed Therapy for Oligometastatic Prostate Cancer Recurrence: A Prospective, Randomized, Multicenter Phase II Trial (STOMP), "Outcomes of Observation vs Stereotactic Ablative Radiation for Oligometastatic Prostate Cancer (ORIOLE)," and "Stereotactic ablative radiotherapy versus standard of care palliative treatment in patients with oligometastatic cancers (SABR-COMET)":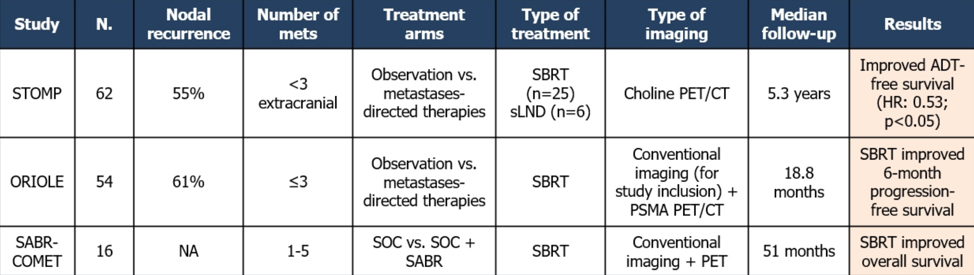
Dr. Briganti specifically highlighted the ORIOLE trial5, which was designed to determine if stereotactic ablative radiotherapy improves oncologic outcomes in men with oligometastatic prostate cancer. In this phase II trial, there were 54 men with 1-3 metastases with conventional imaging randomized 2:1 to receive stereotactic ablative radiotherapy or observation, with a primary outcome of progression at 6 months by PSA level increase (all patients received a PSMA PET/CT at enrollment). Progression at 6 months occurred in 7 of 36 patients (19%) receiving stereotactic ablative radiotherapy and 11 of 18 patients (61%) undergoing observation (p = 0.005). Furthermore, treatment with stereotactic ablative radiotherapy improved median PFS (not reached vs 5.8 months; HR 0.30, 95% CI 0.11-0.81). Also, the total consolidation of PSMA radiotracer-avid disease decreased the risk of new lesions at six months (16% vs 63%, p = 0.006).
Dr. Briganti highlighted that we must be judicious in who we select for a salvage lymph node dissection. In his opinion, the optimal candidate is a patient with a longer time to biochemical recurrence, low PSA, Gleason Grade Group 1-4, and 1-2 PET-positive pelvic lymph nodes.
Dr. Briganti concluded his presentation with the following remarks:
- Early use of PSMA PET/CT is associated with high rates of nodal detection
- The benefit of finding early nodal dissemination in the primary setting is unknown (despite treatment change)
- In the recurrent setting, the evidence is accumulating supporting the role of early non-systematic treatment
- The impact on hard clinical endpoints still needs to be demonstrated
- It is likely that combination treatments will change clinical outcomes
Presented by: Alberto Briganti, IRCCS San Raffaele Scientific Institute, Milan, Italy
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, Augusta, GA, Twitter: @zklaassen_md, at the Virtual 2020 EAU Annual Meeting #EAU20, July 17-19, 2020.
References:
- Luiting HB, van Leeuwen PJ, Busstra MB, et al. Use of gallium-68 prostate-specific membrane antigen positron-emission tomography for detecting lymph node metastases in primary and recurrent prostate cancer and location of recurrence after radical prostatectomy: An overview of the current literature. BJU Int 2020;125:206-215.
- Hofman MS, Lawrentschuk N, Francis, RJ, et al. Prostate-specific membrane antigen PET-CT in patients with high-risk prostate cancer before curative-intent surgery or radiotherapy (proPSMA): A prospective, randomized, multicentre study. Lancet 2020 Apr 11;395(10231):1208-1216.
- Fossati N, Scarcella S, Gandaglia G, et al. Underestimation of Positron Emission Tomography/Computerized Tomography in Assessing Tumor Burden in Prostate Cancer Nodal Recurrence: Head-to-Head Comparison of 68Ga-PSMA and 11C-Choline in a Large, Multi-Institutional Series of Extended Salvage Lymph Node Dissections. J Urol 2020 Aug;204(2):296-302.
- Han S, Woo S, Kim YJ, et al. Impact of 68Ga-PSMA PET on Management of Patients with Prostate Cancer: A Systematic Review and Meta-Analysis. Eur Urol 2018 Aug;74(2):179-190.
- Phillips R, Shi WY, Deek M, et al. Outcomes of Observation vs Stereotactic Ablative Radiation for Oligometastatic Prostate Cancer: The ORIOLE Phase 2 Randomized Clinical Trial. JAMA Oncol 2020 Mar 26;6(5):650-659.


