(UroToday.com) The joint session of the European Association of Urology and the Urological Society of Australia and New Zealand at the 2021 European Association of Urology annual meeting included a presentation by Dr. Peter Bostrom discussing the role of adjuvant radiotherapy following radical prostatectomy in men with high-risk disease.
Dr. Bostrom notes that there are several risk factors that must be taken into account when assessing a patient’s risk for biochemical recurrence/consideration for adjuvant radiotherapy, including (i) pT stage, (ii) surgical margins, (iii) Gleason score, (iv) pN stage, (v) post-operative PSA, (vi) comorbidity status, and (vii) immediate functional recovery after surgery. In an assessment of 22,843 patients from 1992-2017 at the Martini Clinic,1 over a median follow-up of 68 months, the most favorable 20-year survival rates were exhibited in NCCN low risk (78.7% BCR-free, 96.8% MFS, 90.1% CSS) and pT2, GGG 1 to 2, R0 patients (83.1% BCR-free, 96.7% MFS, 92.6% CSS). Furthermore, the lowest 10-year CSS (69.8%) was exhibited in pT3b, GGG 4 to 5, R1 patients.
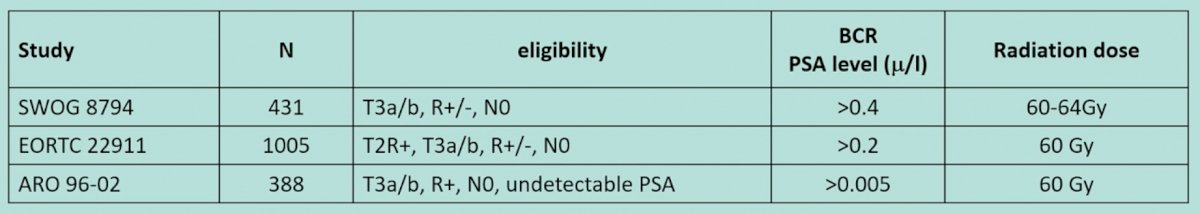
The available evidence assessing adjuvant radiotherapy comes from several trials including the EORTC 22911, SWOG 8794, ARO 96-02, and the Finnprostata-10 trials. For the first three of the aforementioned trials, the eligibility criteria are as follows:
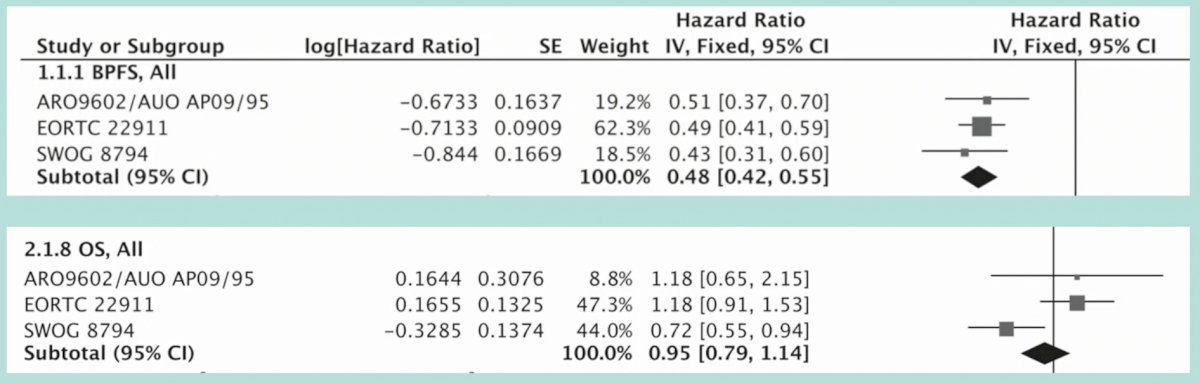
In a meta-analysis of these three trials,2 adjuvant radiotherapy significantly improved biochemical progression-free survival (HR 0.48, 95% CI 0.42-0.55), but did not improve overall survival (HR 0.95, 95% CI 0.79-1.14):
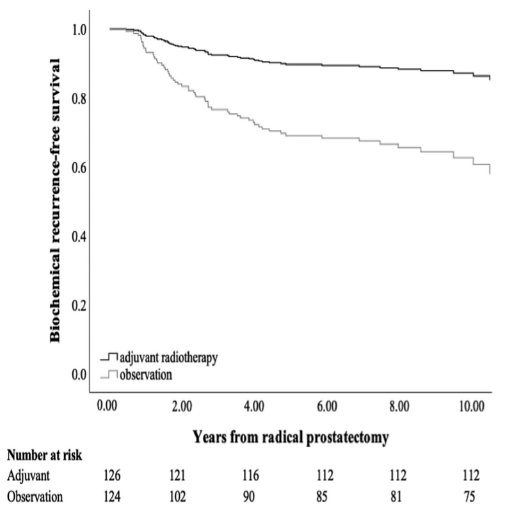
Dr. Bostrom then discussed in detail the FinnProstate-10 trial, a trial that he was part of, which was published in 2019 in European Urology.3 This trial was a randomized, open-label, parallel-group trial, including 250 patients enrolled between April 2004 and October 2012 in eight Finnish hospitals, with pT2 with positive margins or pT3a, pN0, M0 cancer without seminal vesicle invasion. The intervention arm included 126 patients that received 66.6 Gy of adjuvant radiotherapy and the primary endpoint was biochemical recurrence-free survival. The median follow-up time for patients who were alive when the follow-up ended was 9.3 years in the adjuvant group and 8.6 years in the observation group. There were 15 biochemical recurrence events in the adjuvant arm and 43 events in the control arm (HR 0.30, 016-0.53), and the 10-yr survival for biochemical recurrence was 82% in the adjuvant group and 61% in the observation group (HR 0.26, 95% CI 0.14-0.48, p<0.001):
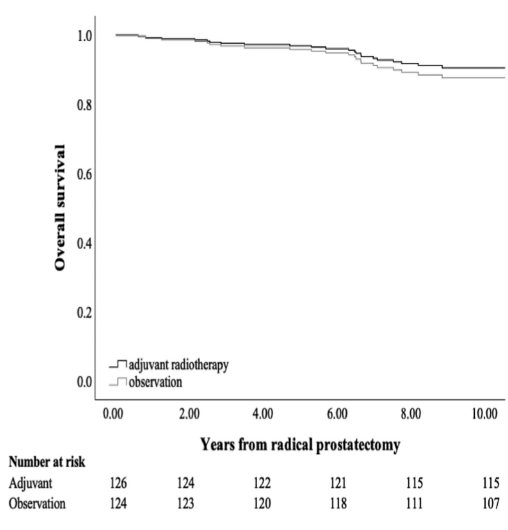
Overall survival was 92% in the adjuvant arm and 87% in the observation arm (HR 0.69, 95% CI 0.29-1.60, p=0.4):
Out of the 43 patients with biochemical recurrence in the observation group, 37 patients received salvage radiotherapy. With regards to adverse events, in the adjuvant group, 56% experienced grade 3 adverse events, compared to only 40% in the observation group (p=0.016).
Dr. Bostrom notes that ultrasensitive PSA is more commonly available today than when most of the adjuvant radiotherapy trials were accruing patients. Based on the RAVES, RADICALS, and GETUG-AFU trials, there was no difference in biochemical recurrence rates between patients receiving adjuvant versus early salvage radiotherapy, however longer follow-up data are needed. The current EAU guidelines state that we should only offer adjuvant IMRT plus IGRT to high-risk patients (pN0) with at least two out of three high-risk features (ISUP grade group 4-5, pT3 +/- positive margins).
Dr. Bostrom notes that there are several open questions that remain to be answered:
- How do we manage node-positive cases?
- How do we management PSA persistence after surgery?
- How/when do we use ADT with radiotherapy in the adjuvant/salvage setting?
- What is the utility of advanced imaging, specifically PSMA/PET?
- Is there a subpopulation of high-risk cases which benefit from adjuvant radiotherapy compared to ultrasensitive PSA and PSMA-PET guided low-PSA threshold salvage radiotherapy?
Dr. Bostrom concluded with the following take-home messages:
- Adjuvant radiotherapy significantly improves biochemical recurrence-free survival rates
- Adjuvant radiotherapy is associated with significantly more toxicity than salvage radiotherapy
- Adjuvant radiotherapy should be discussed with men with very high-risk of recurrence
Presented by: Peter J. Bostrom, MD, PhD, University of Turku and Turku University Hospital, Turku, Finland
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.
References:
- Wurnschimmel C, Wenzel M, Wang N, et al. Radical prostatectomy for localized prostate cancer: 20-year oncological outcomes from a German high-volume center. Urol Oncol. 2021 Jun 3;S1078-1439(21)00188-5.
- Shaikh MP, Alite F, Wu MJ, et al. Adjuvant radiotherapy versus wait-and-see strategy for pathologic T3 or margin-positive prostate cancer: A Meta-Analysis. Am J Clin Oncol. 2018 Aug;41(8):730-738.
- Hackman G, Taari K, Tammela TL, et al. Randomized trial of adjuvant radiotherapy following radical prostatectomy versus radical prostatectomy alone in prostate cancer patients with positive margins or extracapsular extension. Eur Urol. 2019 Nov;76(5):586-595.


