(UroToday.com) The joint session of the European Association of Urology and the Confederacion Americana de Urologia included a session discussing the surgical treatment of lymph node recurrences after radical prostatectomy. Dr. Piet Ost from Ghent University Hospital in Belgium took the pro radiotherapy approach for his presentation.
Dr. Ost notes that a familiar story is that a patient undergoes a radical prostatectomy, has a PSA recurrence for which he receives salvage radiotherapy, and subsequently has a rising PSA with negative conventional imaging, but a positive PSMA PET recurrence in the pelvis. There are several treatment options for the patient at this time:
- Observation with ADT at time of progression
- Immediate ADT
- ADT + docetaxel
- Metastasis directed therapy (any surgical or radiotherapy option)
- Metastasis directed therapy + systemic therapy of choice
Dr. Ost emphasized that patients with PET-detected nodal recurrences live for many years and they generally would rather live longer without long-term side effects. Data from the salvage lymph node dissection literature suggests that after 12 years from their salvage lymph node dissection, more than 60% of patients are still alive.
When considering whole pelvis radiotherapy versus standard extended salvage lymph node dissection, it is important to consider the areas treated, with broader coverage provided by a whole pelvis radiotherapy approach:1

The Oligopelvis-GETUG P07 trial was first presented at the 2020 GU ASCO meeting and will be published soon in European Urology. This was a multicenter phase II trial of combined salvage radiotherapy and hormone therapy (6 months of ADT) in oligorecurrent pelvic node relapsed prostate cancer. The main objective of this trial was to assess biochemical-clinical failure defined by a cluster of events including PSA progression (≥25 % and ≥ 2 ng/ml above the nadir) or clinical evidence of local or metastatic progression or post-treatment initiation of hormonal therapy or prostate cancer-related death. Among 67 patients, at 2 and 3 years, 73.1 and 45.9% of patients achieved a persisting complete response, respectively. After a median follow-up of 34 months, the 2-year progression-free survival rate was 77.6%, and the median progression-free survival was 40.1 months. With regards to adverse effects of treatment, grade 2+ two-year urinary and intestinal toxicity was only 10% and 2%, respectively.
Previous work from Dr. Ost’s group sought to compare outcome and toxicity between stereotactic body radiotherapy and elective nodal radiotherapy, with a primary endpoint of metastasis-free survival. In this multi-institutional study of 506 men, 309 received stereotactic body radiotherapy and 197 received elective nodal radiotherapy.2 Elective nodal radiotherapy was associated with fewer nodal recurrences compared with stereotactic body radiotherapy (p < 0.001):

In a multivariable analysis, patients with one lymph node at recurrence had longer adjusted metastasis free survival after elective nodal radiotherapy (HR 0.50, 95% CI 0.30-0.85, p = 0.009). Additionally, late toxicity was higher after elective nodal radiotherapy compared with that after stereotactic body radiotherapy (16% vs. 5%, p < 0.01):

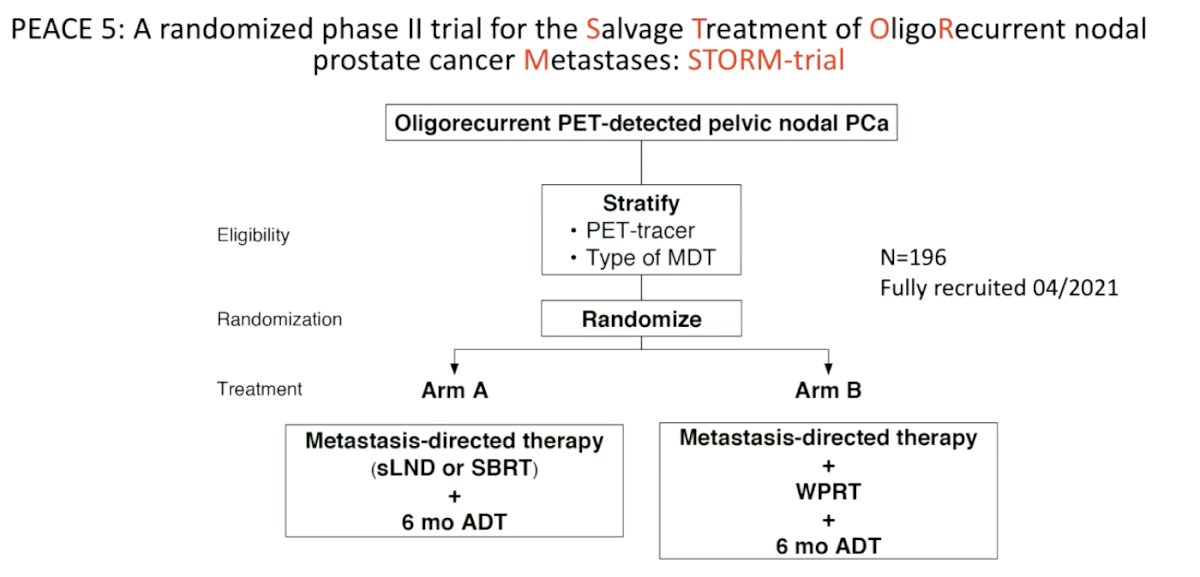
Dr. Ost highlights that we are looking forward to the STORM trial (which has completed accrual, but will take 2 years for the first clinical outcomes to be reported), which is highlighted as follows:
Dr. Ost concluded his presentation with the following take-home messages:
- Whole pelvis radiotherapy covers both visible and invisible recurrences to a larger extent as compared to surgery
- Toxicity seems to be less than compared to surgery
- Pattern of relapse of whole pelvis radiotherapy is predominantly outside of the pelvis
- Approximately 50% of patients still relapse within 2 years, indicating that we likely need local + systemic therapy to make a meaningful difference
Presented by: Piet Ost, MD, PhD, Ghent University Hospital, Ghent, Belgium
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.
References:
- De Bruycker A, De Bleser E, Decaestecker K, et al. Nodal oligorecurrent prostate cancer: Anatomic pattern of possible treatment failure in relation to elective surgical and radiotherapy treatment templates. Eur Urol. 2019 May;75(5):826-833.
- De Bleser E, Jereczek-Fossa BA, Pasquier D, et al. Metastasis-directed therapy in treating nodal oligorecurrent prostate cancer: A multi-institutional analysis comparing the outcome and toxicity of stereotactic body radiotherapy and elective nodal radiotherapy. Eur Urol. 2019 Dec;76(6):732-739.


