Dr. Carlsson began her talk setting the stage for active surveillance. She reviewed the basic epidemiology of prostate cancer highlighting that it is generally a non-lethal disease in the majority of men. The incidence of prostate cancer is 7-fold higher than mortality. Unfortunately, the active treatment for prostate cancer affects several domains of men’s quality of life (QoL) whereas active surveillance either has limited or no effect on these aspects. For this reason, active surveillance is generally preferred if it is safe and does not compromise cancer care.
She then highlighted her work at Memorial Sloan-Kettering looking at outcomes of active surveillance for GG1 and GG2 prostate cancer.1,2
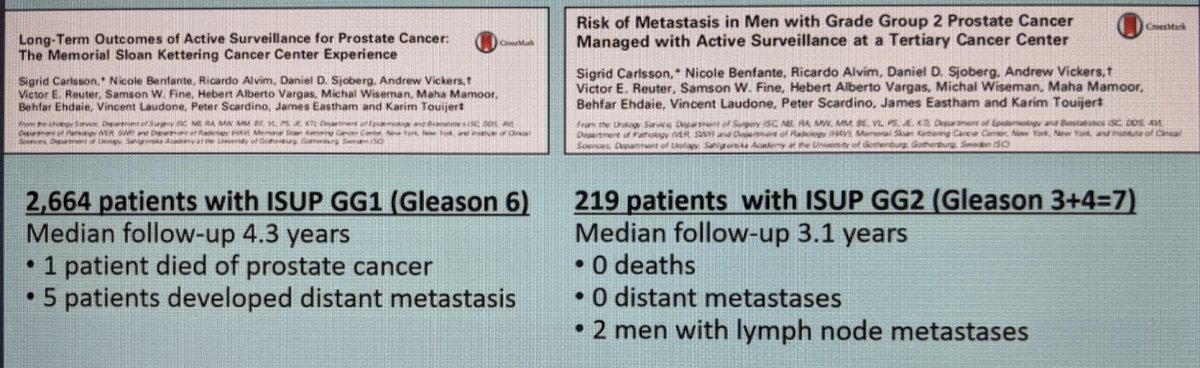
Clearly, while the cohort of men with intermediate-risk prostate cancer is smaller and likely well selected, they have comparable outcomes to men with GG1 disease. She notes that half the men with GG2 disease remained untreated at 10 years, thereby avoiding active treatment and its QoL impact.
In multiple studies, there is evidence that the utilization of AS for low and intermediate-risk prostate cancer is increasing. From the study by Loeb et al.,3 ~20% of men on AS in Sweden had intermediate-risk disease.
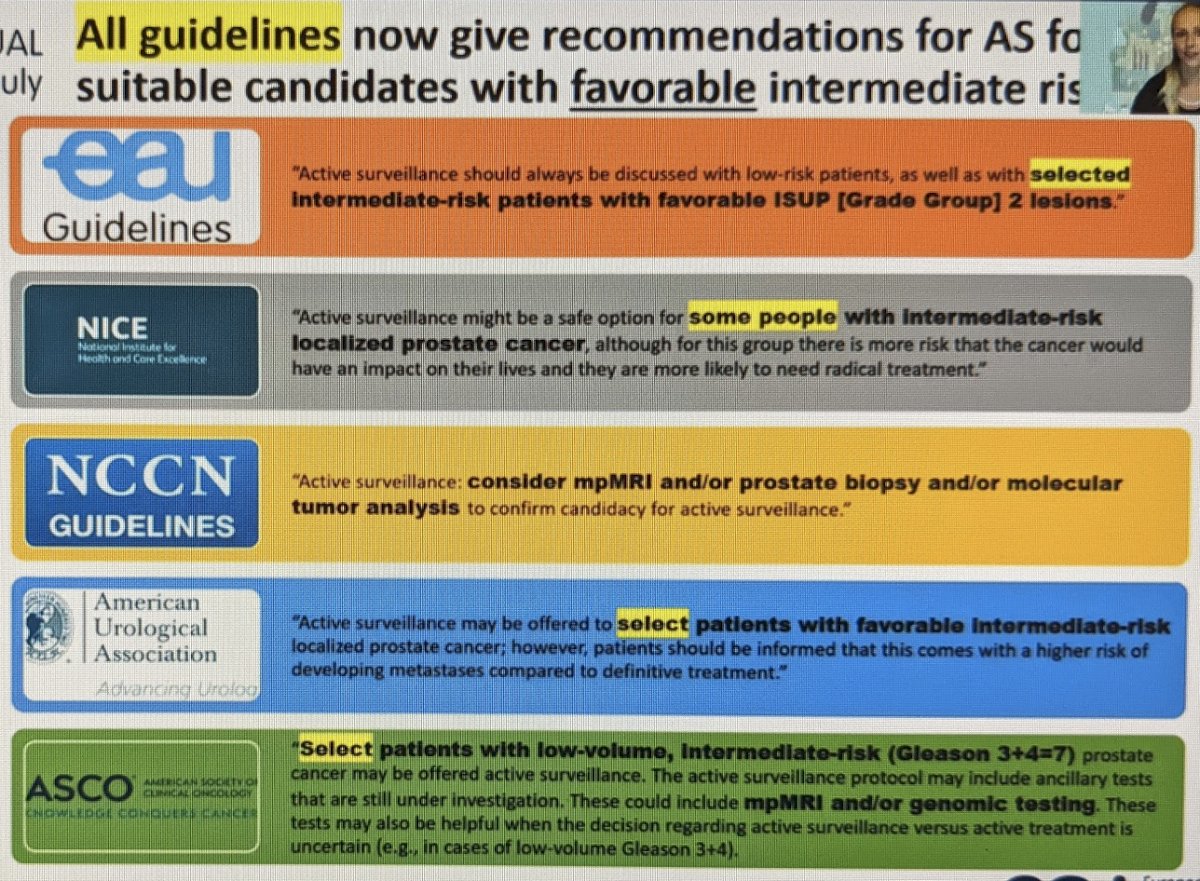
She also highlighted the fact that all the major guidelines now get recommendations for active surveillance for suitable candidates with favorable intermediate-risk prostate cancer but emphasized the importance of patient selection. Specifically, they recommend surveillance only if the patient has favorable intermediate-risk prostate cancer, low-volume pattern 4 disease, low PSAD, mpMRI, and molecular markers. The diagram below summarized the guideline recs:
There are 4 RCTs and 14 observational studies that provide evidence on oncologic outcomes of expectant management (active monitoring or active surveillance) for intermediate-risk PCa.
In ProtecT,4 there were few prostate cancer deaths at 10 years and no differences by treatment arm or disease risk. Of the 111 men with Gleason 7 on active monitoring, 5 died of prostate cancer – but this may have included some GG3 disease.
There have been 14 series that have reported on active surveillance for men with favorable intermediate-risk PCa. In a review that is pending publication, she notes that several of those series report no metastases and no deaths. Others in those series report equivalent survival rates to low-risk prostate cancer men. (Carlsson S et al. BMC Urology, submitted).
In the Sunnybrook series,5 the presence of pattern 4 disease was the major driver of the high metastatic rate. 15-year metastases-free survival dropped from 94% for GG1 disease to 83.6% in men with GG2 disease and 63.2% in men with GG3 disease. The importance of the percentage of pattern 4 has been validated on radical prostatectomy series, comparing biopsy to prostatectomy pathology. It has also been demonstrated to be incrementally predictive of recurrence-free survival after prostatectomy. (Sauter et al. EU 2015, Epstein et al. 2015, Cole et al. JUrol 2016). Her groups’ work at MSKCC demonstrated that quantification of Gleason pattern 4 on biopsy (via core length) was also correlated to adverse pathology at the time of RP.6
She lastly notes that she feels that the outcomes of Active surveillance for intermediate-risk prostate cancer in modern series may be even better than prior series for a few reasons:
- Active surveillance is different than the “watchful waiting” or “active monitoring” the older series
- MRI is used to identify high-grade cancers earlier
- Genomic markers have been introduced
- We use 12 core biopsy rather than a sextant biopsy
- Great modification: some of our GG2 used to be GG1 on old studies
Her conclusions are as follows:
- Active surveillance definitely has a role for intermediate-risk prostate cancer
- it is a safe initial management strategy at dedicated cancer centers for carefully selected men with GG2 prostate cancer who are monitored closely according to well-defined active surveillance criteria
- men with intermediate-risk disease being considered for active surveillance should be counseled about the relative lack of evidence on long-term oncologic outcomes
At this point, Dr. Robert took over to argue against AS for GG2 prostate cancer. He addresses this in point-by-point fashion.
He first noticed that most of the large cohort series that support active surveillance and published their protocols do not include GG2 prostate cancer, except the series by Bul et al.7
When the main cohort studies are pooled there are very few patients with GG2 prostate cancer.
Next, he notes the misclassification rates at the time of biopsy. He notes that amongst 10,089 men with GG2 prostate cancer (PSA < 10, cT1c-2a, <50% core positive), approximately 30.2% were upgraded or upstaged at the time of radical prostatectomy. Sayyid et al.,8 using SEER, found that in men with GG2 on prostate biopsy who underwent radical prostatectomy, there was a 13.3% upgrading risk. So, he feels that with our current diagnostic modalities there is a high rate of under staging of Intermediate risk prostate cancer.
He next notes the lack of level 1 evidence to support Active surveillance. He notes that Dr. Carlsson’s use of the ProtecT data is flawed, as active monitoring is not the same as active surveillance. In that study, while there may not have been as many cancer deaths, there were high metastases rates in men on active monitoring (6% vs. 2.6%).
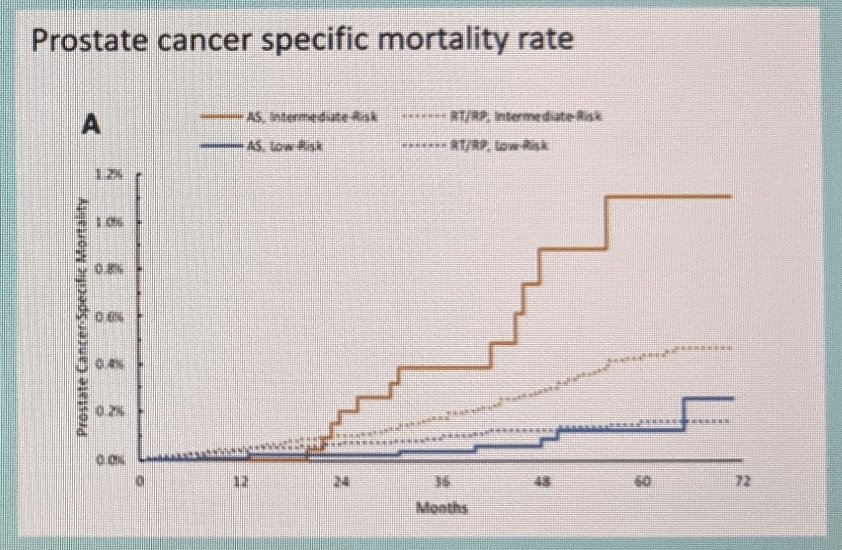
He lastly highlights again the Sunnybrook series.5 This corresponds with the ProtecT data in that the rate of metastatic spread while on AS was much higher for men with GG2 disease than men with GG1 disease (~11% absolute difference at 15 years). He then notes that the opportunity for cure may be lost – data by Abern et al.9 suggests that delayed prostatectomy is associated with higher biochemical recurrence, particularly for patients with GG2 disease. Butler et al.10 also noted that active surveillance was associated with a -[=]\slightly higher and statistically significant increase in 5-year prostate cancer specific mortality compared with active treatment – seen in the KM curve below.
Based on this, he concludes that:
1. Active surveillance for GG2 prostate cancer remains questionable
- there is a significant amount of misclassification
- there’s no high-level evidence and very few retrospective data
- there’s worst evolution after deferred treatment
2. Patient selection is key
- role MRI remains investigational
- it’s preferable to include these patients in clinical studies at this time
Presented by:
Pro: Sigrid Carlsson, MD, Ph.D., MPH, Memorial Sloan Kettering Cancer Center, New York, NY
Con: Grégoire Robert, MD, PhD, Department of Urology, CHU Bordeaux, University of Bordeaux, Bordeaux, France
Written by: Thenappan (Thenu) Chandrasekar, MD – Urologic Oncologist, Assistant Professor of Urology, Sidney Kimmel Cancer Center, Thomas Jefferson University, @tchandra_uromd on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.
References:
- Carlsson S, Benfante N, Alvim R, Sjoberg DD, Vickers A, Reuter VE, Fine SW, Vargas HA, Wiseman M, Mamoor M, Ehdaie B, Laudone V, Scardino P, Eastham J, Touijer K. Long-Term Outcomes of Active Surveillance for Prostate Cancer: The Memorial Sloan Kettering Cancer Center Experience. J Urol. 2020 Jun;203(6):1122-1127. doi: 10.1097/JU.0000000000000713. Epub 2019 Dec 23. PMID: 31868556; PMCID: PMC7480884.
- Carlsson S, Benfante N, Alvim R, Sjoberg DD, Vickers A, Reuter VE, Fine SW, Vargas HA, Wiseman M, Mamoor M, Ehdaie B, Laudone V, Scardino P, Eastham J, Touijer K. Long-Term Outcomes of Active Surveillance for Prostate Cancer: The Memorial Sloan Kettering Cancer Center Experience. J Urol. 2020 Jun;203(6):1122-1127. doi: 10.1097/JU.0000000000000713. Epub 2019 Dec 23. PMID: 31868556; PMCID: PMC7480884.
- Loeb S, Folkvaljon Y, Curnyn C, Robinson D, Bratt O, Stattin P. Uptake of Active Surveillance for Very-Low-Risk Prostate Cancer in Sweden. JAMA Oncol. 2017 Oct 1;3(10):1393-1398. doi: 10.1001/jamaoncol.2016.3600. PMID: 27768168; PMCID: PMC5559339.
- Hamdy FC, Donovan JL, Lane JA, Mason M, Metcalfe C, Holding P, Davis M, Peters TJ, Turner EL, Martin RM, Oxley J, Robinson M, Staffurth J, Walsh E, Bollina P, Catto J, Doble A, Doherty A, Gillatt D, Kockelbergh R, Kynaston H, Paul A, Powell P, Prescott S, Rosario DJ, Rowe E, Neal DE; ProtecT Study Group. 10-Year Outcomes after Monitoring, Surgery, or Radiotherapy for Localized Prostate Cancer. N Engl J Med. 2016 Oct 13;375(15):1415-1424. doi: 10.1056/NEJMoa1606220. Epub 2016 Sep 14. PMID: 27626136.
- Musunuru HB, Yamamoto T, Klotz L, Ghanem G, Mamedov A, Sethukavalan P, Jethava V, Jain S, Zhang L, Vesprini D, Loblaw A. Active Surveillance for Intermediate Risk Prostate Cancer: Survival Outcomes in the Sunnybrook Experience. J Urol. 2016 Dec;196(6):1651-1658. doi: 10.1016/j.juro.2016.06.102. Epub 2016 Aug 26. PMID: 27569437.
- Dean LW, Assel M, Sjoberg DD, Vickers AJ, Al-Ahmadie HA, Chen YB, Gopalan A, Sirintrapun SJ, Tickoo SK, Eastham JA, Scardino PT, Reuter VE, Ehdaie B, Fine SW. Clinical Usefulness of Total Length of Gleason Pattern 4 on Biopsy in Men with Grade Group 2 Prostate Cancer. J Urol. 2019 Jan;201(1):77-82. doi: 10.1016/j.juro.2018.07.062. PMID: 30076908; PMCID: PMC6786261.
- Bul M, van den Bergh RC, Zhu X, Rannikko A, Vasarainen H, Bangma CH, Schröder FH, Roobol MJ. Outcomes of initially expectantly managed patients with low or intermediate risk screen-detected localized prostate cancer. BJU Int. 2012 Dec;110(11):1672-7. doi: 10.1111/j.1464-410X.2012.11434.x. Epub 2012 Aug 29. PMID: 22928973.
- Sayyid RK, Reed WC, Benton JZ, Lodh A, Woodruff P, Lambert JH, Terris MK, Wallis CJD, Klaassen Z. Pathologic upgrading in favorable intermediate risk active surveillance patients: Clinical heterogeneity and implications for active surveillance decision. Urol Oncol. 2021 Mar 22:S1078-1439(21)00079-X. doi: 10.1016/j.urolonc.2021.02.017. Epub ahead of print. PMID: 33766466.
- Abern MR, Aronson WJ, Terris MK, Kane CJ, Presti JC Jr, Amling CL, Freedland SJ. Delayed radical prostatectomy for intermediate-risk prostate cancer is associated with biochemical recurrence: possible implications for active surveillance from the SEARCH database. Prostate. 2013 Mar;73(4):409-17. doi: 10.1002/pros.22582. Epub 2012 Sep 19. PMID: 22996686.
- Butler SS, Mahal BA, Lamba N, Mossanen M, Martin NE, Mouw KW, Nguyen PL, Muralidhar V. Use and early mortality outcomes of active surveillance in patients with intermediate-risk prostate cancer. Cancer. 2019 Sep 15;125(18):3164-3171. doi: 10.1002/cncr.32202. Epub 2019 May 31. PMID: 31150125.


