In this study, the investigators aimed to assess the predictive accuracy, the best cut-off value, and the clinical impact of the recently published nomogram through an external validation in a multicenter cohort.
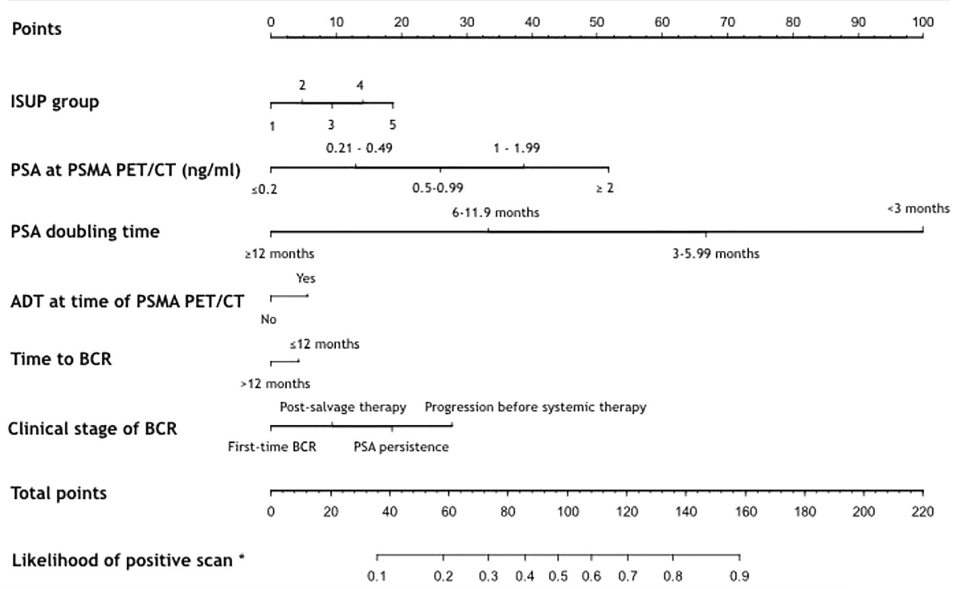
This study retrospectively enrolled 1,639 prostate cancer patients from six institutions with confirmed biochemical recurrence after radical treatment for prostate cancer that underwent 68Ga-PSMA PET/CT to identify recurrence. First, the detection rate of 68Ga-PSMA PET/CT was evaluated. Second, a multivariable logistic regression model was used to evaluate predictors for 68Ga-PSMA PET/CT positivity. External validation was performed using the same regression coefficients of the previous nomogram: ISUP group, PSA at the time of PET/CT scan, PSA doubling time, ongoing ADT, time to biochemical recurrence (≤12 months vs >12 months), and clinical setting (First BCR [group 1], BCR after salvage therapy [group 2], PSA persistence [group 3]and advanced-stage prostate cancer before second-line systemic therapies [group 4]). The performance characteristics of the model were assessed by quantifying predictive accuracy, according to model calibration, in order to graphically investigate the extent of overestimation or underestimation. Finally, decision-curve analysis was performed to evaluate the net benefit of the proposed nomogram.
The median PSA at PSMA PET/CT was 0.78 ng/ml (IQR 0.4- 1.72). In the external cohort, the overall detection rate of PSMA-PET/CT was 53.8% versus 51.2% in the original population. 68Ga-PSMA PET/CT overall detection rate was 43.5 %, 57.3 %, 59% and 85.9 % in group 1,2,3 and 4, respectively (p<0.001). At multivariable analysis ISUP grade group (ISUP 5 OR 1.76), PSA at PET/CT (0.5 – 0.99ng/mL OR 3.64; 1 – 1.99 ng/mL OR 6.27; >2ng/mL OR 13.48), PSA doubling time (6-11.9 months OR 2.84; 3-5.9 months OR 9.12; <3 months OR 14.21) and the clinical setting (group 2, OR 1.37 and group 4, OR 5.13) were found to be independent predictors of positive 68Ga-PSMA PET/CT results (all p≤0.02). The predictive accuracy of the nomogram in the external validation was identical to that reported in the original model (82% versus 82%, respectively). The resulting nomogram showed an optimal calibration curve (mean absolute error 0.019). The decision-curve analysis depicted a clinical net-benefit for risk thresholds higher than 20%:
Dr. Bianchi concluded the presentation by emphasizing that the proposed nomogram showed good predictive performance in the external validation population and could help clinicians choose which patients could benefit most from 68Ga-PSMA PET/CT.
Presented By: Lorenzo Bianchi, MD, FEBU, Urologist Sant’Orsola-Malpighi Hospital, University of Bologna
Written By: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.
References:


