Analysis was limited to patients that were diagnosed with nodal-only recurrent prostate cancer via PSMA-PET/CT. Salvage lymph node dissection was performed via open approach, and for salvage lymph node radiation therapy, radiotherapy dose regimens were normo- or slightly hypo-fractionated, with a boost to the PSMA PET-positive local recurrences within prostatic fossa and lymph nodes applied simultaneously. Questionnaires were sent to obtain functional and oncological outcomes, and EORTC QLQ-C30 and PR-25 questionnaires were used to assess HRQOL. Continence status was assessed using daily pad usage and the validated ICIQ-SF questionnaire. Cox regression models were used for multivariable analysis (p<0.05).
There were 138 patients included in the current analysis, including 71 in the salvage lymph node dissection arm and 67 in the salvage lymph node radiation therapy arm:
The median follow-up was 47 months for salvage lymph node radiation therapy patients (IQR 40 – 61), and 33 months for salvage lymph node dissection patients (IQR 20–49; p<0.001). Peri-interventional androgen deprivation therapy (ADT) was administered to 89.6% in the salvage lymph node radiation therapy subgroup and only 5.6% among patients undergoing salvage lymph node dissection (p<0.001). Median ADT duration for salvage lymph node radiation therapy patients was 9 months (IQR 3–21), and 43 patients (65.2%) in the salvage lymph node dissection cohort underwent ADT during follow-up. The biochemical recurrence rate was 40.3% for the salvage lymph node radiation therapy group and 86.4% for the salvage lymph node dissection group (p<0.001). In multivariable analysis, salvage lymph node radiation therapy was confirmed as an independent predictor for increased biochemical recurrence-free survival (RFS; HR 0.08, 95% CI 0.04–0.14, p<0.001). Estimated mean metastasis-free survival (MFS) was 57.6 months (95% CI 51.4 – 63.8) for salvage lymph node radiation therapy patients and 39.5 months (33.4–45.6) for salvage lymph node dissection patients (HR 0.64, 95% CI 0.32-1.31, p=0.222):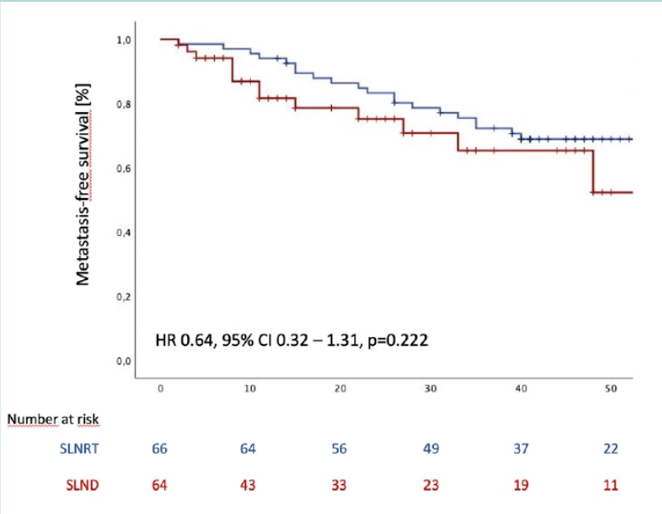
There were no significant differences regarding general HRQOL (QLQ-C30 global health status), daily pad usage, and ICIQ-SF scores between both subgroups: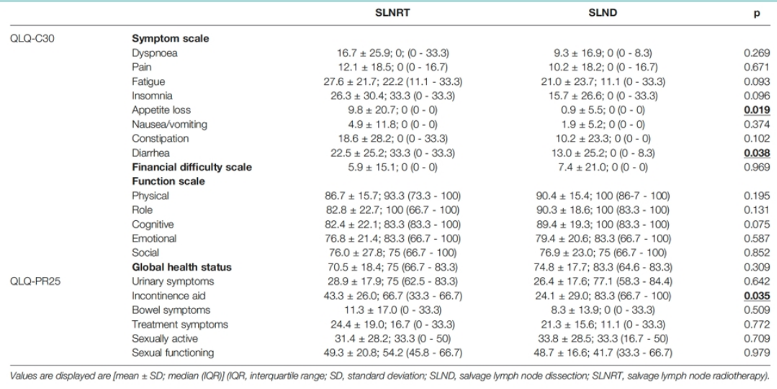
Dr. Kretschmer concluded his presentation with the following take-home messages:
- In a large contemporary series of patients with nodal-only recurrent prostate cancer based on PSMA-PET/CT staging, there was a significantly increased biochemical RFS in patients undergoing salvage lymph node radiation therapy
- There were no significant differences observed in MFS, and functional outcomes, including HRQOL
Presented By: Alexander Kretschmer, MD, LMU Munich, Dept. of Urology, Munich, Germany
Written By: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.


