His first slide has a diagram which he feels is the most important slide of this talk:
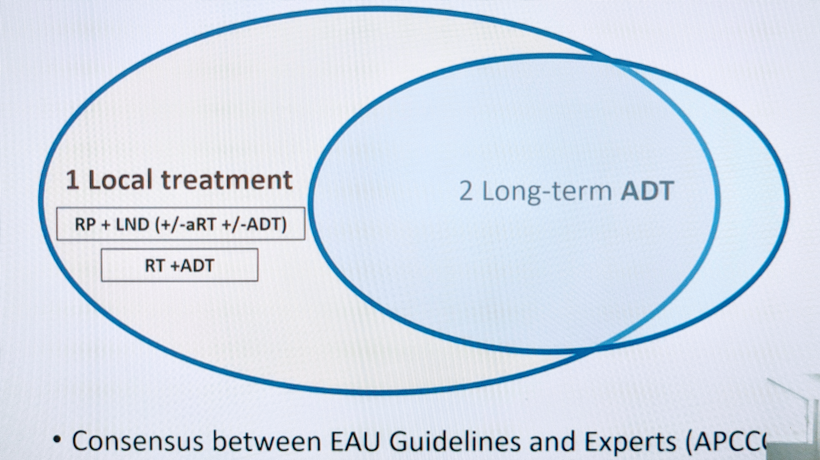
He notes that this depicts the current consensus between EAU guidelines and expert opinion – and basically states that node positive disease should be managed with local therapy and long-term ADT.
He then focuses on the data supporting local therapy. The first is data supporting the use of radiotherapy in the setting of node positive disease. He cites another arm of the STAMPEDE study,1 which compared ADT with radical radiotherapy against ADT alone.
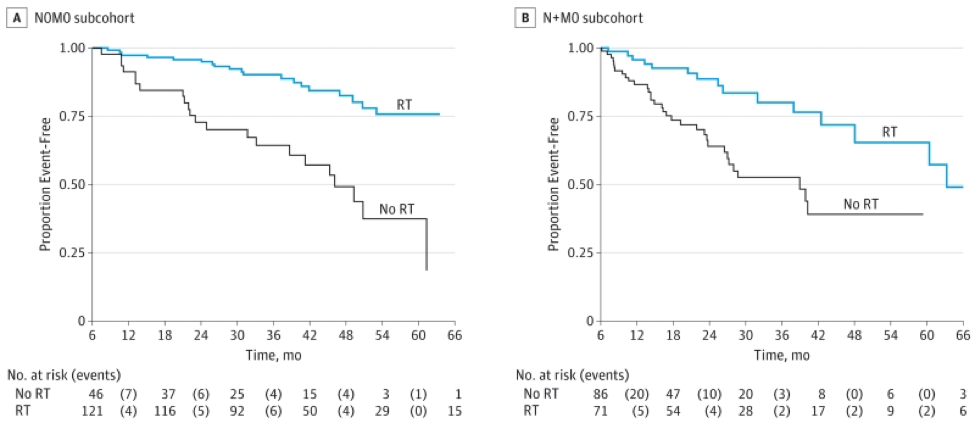
As seen on the right, in the node positive patients, the addition of RT provided significant FFS benefit over ADT alone. This has led to its incorporation into the guidelines.
While similar the Data is lacking for surgery, it can likely be extrapolated. He compares the following two studies to demonstrate the potential benefit of surgery in the setting:
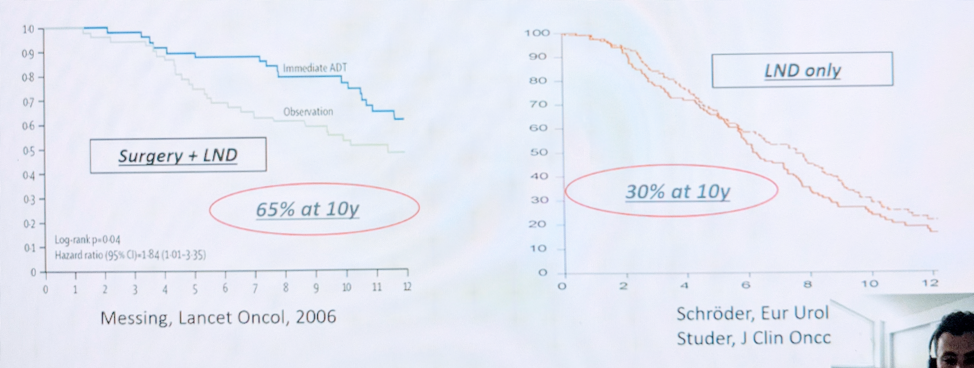
In these two studies, surgery (prostatectomy with LND on the left vs. LND alone on the right) was compared against ADT for node positive patients. The inclusion of radical prostatectomy appeared to confer a survival benefit over ADT alone – and over LND dissection alone!
So, it appears that local therapy is important in this patient population.
As for treatment intensification beyond just ADT, he highlights the James et al. STAMPEDE study,3 the Vale et al.4 meta-analysis, and the Eastham et al.5 B90203 trial to highlight the fact that addition of abiraterone, docetaxel and enzalutamide, respectively, resulted in improved relapse-free survival but not overall survival benefit. They all contributed to additional toxicity without overall survival benefit.
Indeed, at the Advanced Prostate Cancer Consensus Conference 2019, there was not unanimous consensus on treatment intensification –
- For men with newly diagnosed cN1 M0 prostate cancer who are fit, only 59% voted for intensification. 39% recommended ADT alone while 2% voted for no systemic therapy.
- For men receiving adjuvant radiation for pN1 M0 disease, only 34% voted for treatment intensification. 65% suggested ADT alone.
He reminded the audience that the current guidelines in the EAU are to offer patients with cN1 disease a local treatment (either RP with ePLND or EBRT) with long-term ADT. This is a weak recommendation.
His main take-home points are:
1. There is no overall survival benefit from an intensified systemic therapy, only failure free survival
2. The first step to initiate intensification should be any distant metastases on conventional imaging
3. Risk of overtreating the majority of patients and under treating some locally if you intensify systemic therapy
4. Maybe the Abiraterone+RT STAMPEDE N+M0 Sub-group OS analysis (pending) may change this discussion
Presented by: Guillaume Ploussard, MD, PhD, Saint-Jean Languedoc Hospital and Institut Universitaire du Cancer – Oncopole, Toulouse, France
References:
1. Parker CC, James ND, Brawley CD, et al. Systemic Therapy for Advanced or Metastatic Prostate cancer: Evaluation of Drug Efficacy (STAMPEDE) investigators. Radiotherapy to the primary tumour for newly diagnosed, metastatic prostate cancer (STAMPEDE): a randomised controlled phase 3 trial. Lancet. 2018 Dec 1;392(10162):2353-2366. doi: 10.1016/S0140-6736(18)32486-3. Epub 2018 Oct 21. PMID: 30355464; PMCID: PMC6269599.
2. Messing EM, Manola J, Yao et al.; Eastern Cooperative Oncology Group study EST 3886. Immediate versus deferred androgen deprivation treatment in patients with node-positive prostate cancer after radical prostatectomy and pelvic lymphadenectomy. Lancet Oncol. 2006 Jun;7(6):472-9. doi: 10.1016/S1470-2045(06)70700-8. PMID: 16750497.
3. James ND, de Bono JS, Spears MR, et al.; STAMPEDE Investigators. Abiraterone for Prostate Cancer Not Previously Treated with Hormone Therapy. N Engl J Med. 2017 Jul 27;377(4):338-351. doi: 10.1056/NEJMoa1702900. Epub 2017 Jun 3. PMID: 28578639; PMCID: PMC5533216.
4. Vale CL, Burdett S, Rydzewska LHM, et al. STOpCaP Steering Group. Addition of docetaxel or bisphosphonates to standard of care in men with localised or metastatic, hormone-sensitive prostate cancer: a systematic review and meta-analyses of aggregate data. Lancet Oncol. 2016 Feb;17(2):243-256. doi: 10.1016/S1470-2045(15)00489-1. Epub 2015 Dec 21. Erratum in: Lancet Oncol. 2016 Feb;17(2):e46. PMID: 26718929; PMCID: PMC4737894.
5. Eastham JA, Heller G, Halabi S, et al. Radical Prostatectomy With or Without Neoadjuvant Chemohormonal Therapy in Localized, High-Risk Prostate Cancer. J Clin Oncol. 2020 Sep 10;38(26):3042-3050. doi: 10.1200/JCO.20.00315. Epub 2020 Jul 24. PMID: 32706639; PMCID: PMC7479762.
6. Gillessen S, Attard G, Beer TM, et al. A. Management of Patients with Advanced Prostate Cancer: Report of the Advanced Prostate Cancer Consensus Conference 2019. Eur Urol. 2020 Apr;77(4):508-547. doi: 10.1016/j.eururo.2020.01.012. Epub 2020 Jan 27. PMID: 32001144.
Read the Opposing Debate:
EAU 2021: cN+ and Systemic Treatment: More than ADT Is Needed as Systemic TTT: Yes!


