(UroToday.com) In this abstract, the authors evaluate the utility of ultra-fast biparametric MRI for prostate cancer detection.
Multiparametric MRI (mpMRI) of the prostate is the imaging modality of choice for the early detection of prostate cancer (PCa) in men with clinical suspicion. However, mpMRI can be costly and time-consuming. mpMRI of the prostate typically has three phases and requires contrast administration.
Recently, biparametric MRI (bpMRI) has been proposed as a valuable alternative to mpMRI to avoid contrast media injection and to reduce scan time and costs, thus increasing MRI availability. The aim of this study was to investigate the diagnostic performance of an abbreviated bpMRI protocol (a–bpMRI: <10 min scan time, no contrast injection, no endorectal coil) for the detection of clinically significant PCa (csPCa).
The study was a retrospective, multi-reader study on 151 men who underwent 3T mpMRI of the prostate followed by transperineal template prostate mapping biopsies, which were performed in all men regardless the MRI findings as part of the PICTURE study.
- For each patient, axial T2 weighted and b2000 diffusion-weighted sequences were extracted from the original mpMRI scan to generate a corresponding a–bpMRI dataset (scan duration: 9 minutes and 13 seconds).
- Three experienced uro–radiologists reviewed and scored a–bpMRI using a 1–to–5 Likert scale, where a score ≥3 means that the lesion is equivocal or suspicious, blinded to clinical information and original mpMRI scores.
The diagnostic accuracy of a–bpMRI was determined based on the results of biopsy using the following definitions of csPCa:
1. Gleason ≥4+3 or cancer core length (CCL) involvement of ≥6mm of any Gleason score (definition 1);
2. Gleason ≥3+4 and/or CCL ≥4 mm (definition 2);
3. presence of any Gleason ≥7.
The individual readers’ results were pooled to define overall a–bpMRI accuracy. Interreader agreement was calculated by percent agreement (PA) and agreement coefficient (AC), including confidence intervals (CI).
Jumping to the results, the median age of included men was 62 years (range: 41–83), median PSA 6.8 ng/ml (range 0.9–28.5).
Demographics:
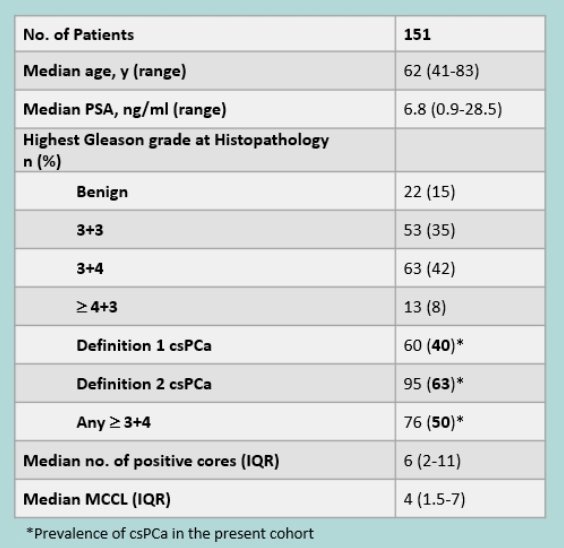
When looking at outcomes, the prevalence of csPCa was 40% using definition 1, 63% using definition 2, and 50% using definition 3.
Using a cut off of Likert 3 for the detection of definition 1 csPCa, sensitivity, specificity, positive predictive value (PPV) and negative predictive value (NPV) of a–bpMRI were 92% (95%CI: 87–96), 48% (95%CI: 42–54), 54% (95%CI: 48–60) and 90% (95%CI: 84–95) respectively; for definition 2 csPCa were 87% (83–91), 65% (57–72), 81% (76–85) and 75% (67–82) respectively; for any Gleason ≥7 were 88% (83–92), 52% (45–59), 65% (59–70) and 81% (73–87) respectively.
These are summarized below:
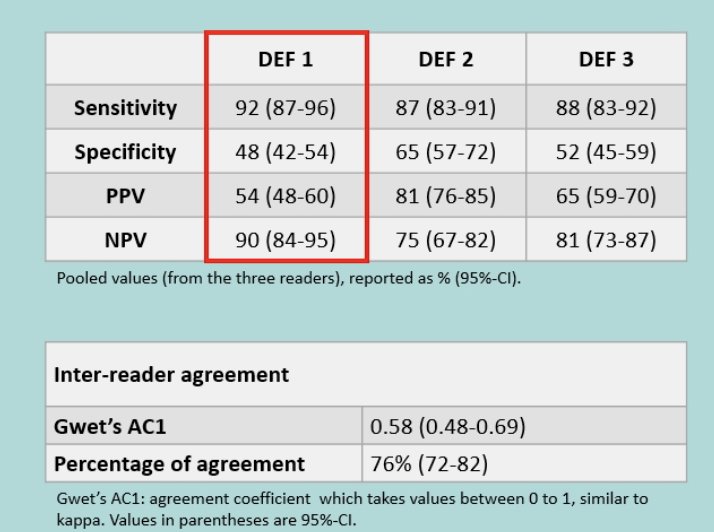
Inter-reader agreement was good (PA: 76% [95%CI: 70-80]; AC: 0.58 [95%CI: 0.48-0.69]).
Based on these results, the authors conclude that ultra-fast biparametric MRI protocols can be performed in <10 min and have high accuracy for the detection of csPCa. In expert hands, the accuracy might approach that of mp-MRI.
Naturally, further studies are warranted before implementation into clinical practice.
However, if implemented, access to prostate MRI would improve and costs would be significantly less.
Presented By: Giorgio Brembilla, Milan, ItalyWritten By: Thenappan (Thenu) Chandrasekar, MD – Urologic Oncologist, Assistant Professor of Urology, Sidney Kimmel Cancer Center, Thomas Jefferson University, @tchandra_uromd on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.


