(UroToday.com) The detection of recurrence and salvage treatment options after primary treatment for prostate cancer session at the European Association of Urology 2021 annual meeting included a presentation by Dr. Daniele Robesti discussing 68Ga-PSMA PET/CT for recurrent prostate cancer after radical prostatectomy. Use of 68Ga-PSMA PET/CT is recommended for prostate cancer re-staging in patients with either PSA persistence or biochemical recurrence after radical prostatectomy. Although this imaging modality is characterized by high sensitivity even at low PSA values, its prognostic implications, as well as the patterns of subsequent progression, have been poorly addressed.
This study retrospectively identified 182 patients who were evaluated with 68Ga-PSMA PET/CT for biochemical recurrence after radical prostatectomy between 2016 and 2020 at IRCCS Ospedale San Raffaele. Imaging during follow-up was performed according to the judgment of each treating physician. Patients were stratified according to PSMA PET/CT into two groups: positive (n=116) versus negative (n=66) scan. Pathological features and salvage treatments were compared. Kaplan-Meier analyses assessed the time from the first PSMA PET/CT to disease progression, and Cox regression analyses assessed the impact of a positive PSMA PET/CT on progression after adjusting for confounders. Per-lesion analysis using Pearson Chi-square assessed the impact of a positive PSMA PET/CT on the location of clinical recurrence after PSMA PET/CT.
Median PSA at PSMA PET/CT scan and time from surgery to biochemical recurrence was 0.7 ng/ml and 49 months, respectively. Overall, 13 (19%) versus 33 (29%) patients experienced disease progression in negative versus positive groups, respectively. No differences were observed for pathologic stage, ISUP group grade, pN status, and rate of salvage radiotherapy and hormonal therapy between the two groups (all p≥0.07). At a median follow-up of 16 months after the first PSMA PET/CT, 46 patients experienced progression. The 3-year progression-free survival rates were 75% vs 40% for negative versus positive PSMA PET/CT scan at the time of biochemical recurrence, respectively:
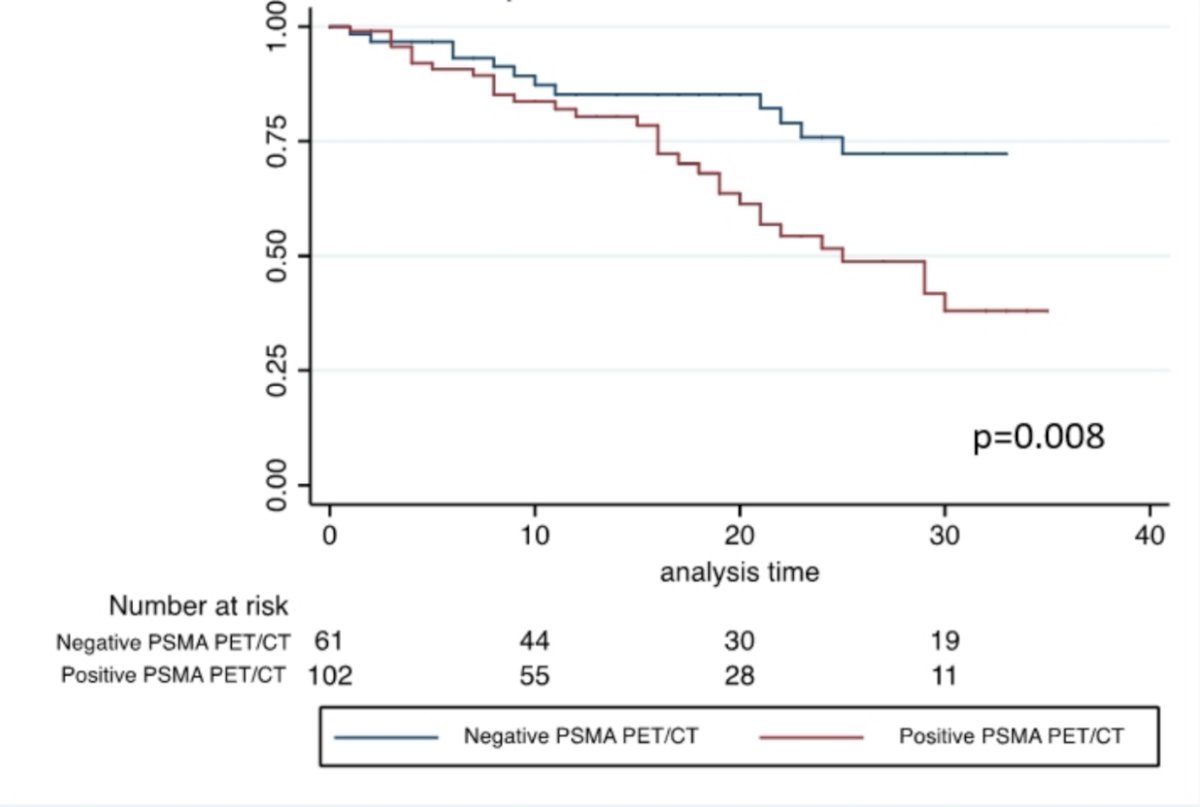
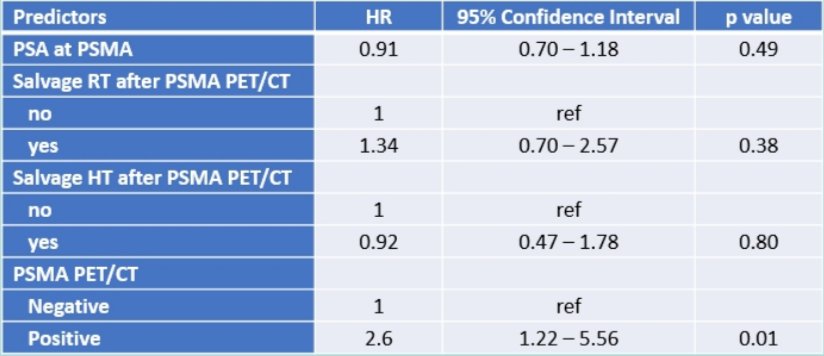
At multivariable analyses, a positive PSMA PET/CT scan was associated with a 2-fold higher risk of progression during follow-up compared to a negative PSMA PET/CT (HR 2.60, 95% CI 1.22-5.56, p=0.01) after adjusting for salvage therapies:
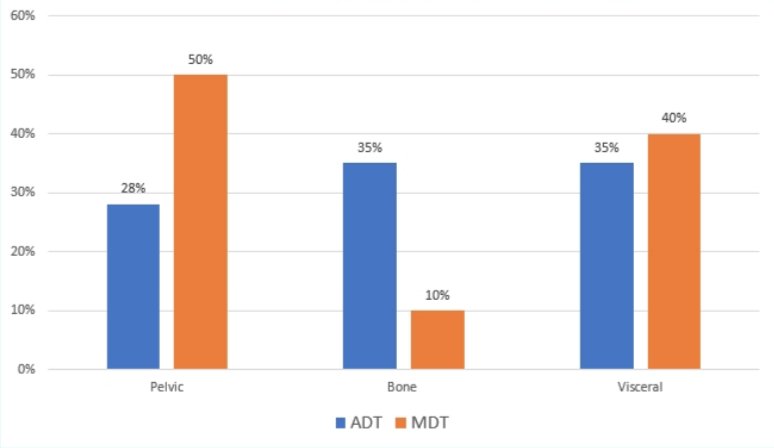
Median time to secondary progression in PSMA negative and positive PET was 44 and 25 months (p=0.006), respectively. In men with negative PSMA (n=66) patterns of recurrence were not influenced by receipt of salvage radiotherapy (no salvage radiotherapy: 37% pelvic, 62% lung versus salvage radiotherapy 30% pelvic, 70% lung). Additionally, in men with positive PSMA PET/CT no differences in terms of site of recurrences were seen between those receiving metastasis directed therapy vs androgen deprivation therapy (ADT: pelvic 28%, bone 35% visceral 35% versus metastasis directed therapy: pelvic 50% bone 10% visceral 40%):
Dr. Robesti concluded his presentation with the following take-home messages:
- The presence of a negative PSMA PET/CT scan represents a protective factor for metastases during follow-up
- Patients with negative PSMA did not show any bony progression during follow-up
- Interestingly, the pattern of recurrence was not influenced by the use of any salvage treatment both in negative and positive PSMA PET patients
- Salvage therapies might impact on time to disease progression but do not alter patterns of prostate cancer dissemination
Presented By: Daniele Robesti, MD, IRCCS Ospedale San Raffaele, Vita-Salute San Raffaele University, Division of Oncology, Unit of Urology, Milan, Italy
Written By: Zachary Klaassen, MD, MSc – Urologic Oncologist, Assistant Professor of Urology, Georgia Cancer Center, Augusta University/Medical College of Georgia, @zklaassen_md on Twitter during the 2021 European Association of Urology, EAU 2021- Virtual Meeting, July 8-12, 2021.


