(UroToday.com) The 2024 European Association of Urology (EAU) annual meeting featured a non-muscle invasive bladder cancer session and a presentation by Dr. Girish Kulkarni discussing the Bladder Utility Symptom Scale (BUSS), a novel tool to measure utilities and quality of life in bladder cancer patients. Bladder cancer and its treatments can have significant impacts on patient quality of life and decision-making. A utility is a preference-based measure of quality of life, anchored from 0 (death) to 1 (full health). To facilitate comparative effectiveness research, a bladder cancer specific tool to measure both quality of life and patient utilities in all phases of bladder cancer care is required. Dr. Kulkarni and his group previously created and validated a 10-item multiple-choice questionnaire to measure quality of life in all phases of bladder cancer care called the Bladder Utility Symptom Scale-Psychometric (BUSS-P). The objective of this study presented at EAU 2024 was to create two distinct algorithms to calculate utilities from BUSS-P responses.
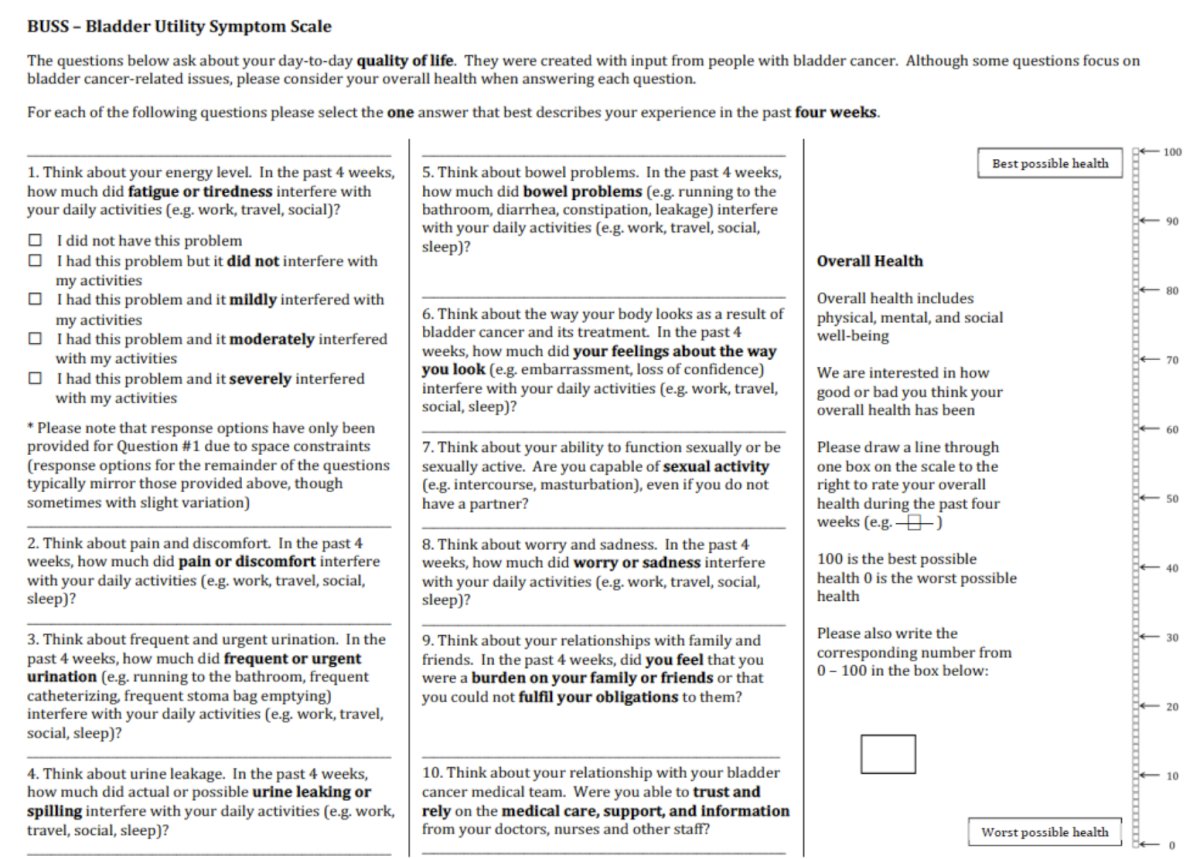
Dr. Kulkarni elicited time tradeoff utilities from 200 bladder cancer patients (from 3 academic institutions – University Health Network, London Health Sciences Centre, and Sunnybrook Health Sciences Centre) and 200 members of the general public during in-person interviews on randomly generated BUSS-P questionnaire response scenarios. The BUSS-P questionnaire is as follows:
Purposeful sampling was used to ensure a proportionate number of non-muscle invasive, muscle invasive, and metastatic bladder cancer patients. The general public sample was recruited proportionate to national age, sex, and income distributions to truly represent community members. Participants first performed a logic and comprehension exercise to ensure they could proceed with the time trade off method. Time trade offs were performed by presenting participants with 13 BUSS-P health states (10 randomly selected + 2 anchor states + a participant’s own state) and a theoretical number of years of life remaining. Participants determined how many years of life they would be willing to sacrifice in order to move to a state of perfect health, where health states resulting in few years sacrificed would result in higher utility values. Bayesian generalized linear multilevel models were used to estimate the impact of each of the 10 BUSS-P attributes to utility which was bound by 0 and 1. Pearson correlation coefficients were calculated between observed and expected model values. Two algorithms to calculate utilities from BUSS-P responses were then generated: one derived from bladder cancer patients and one derived from the general public.
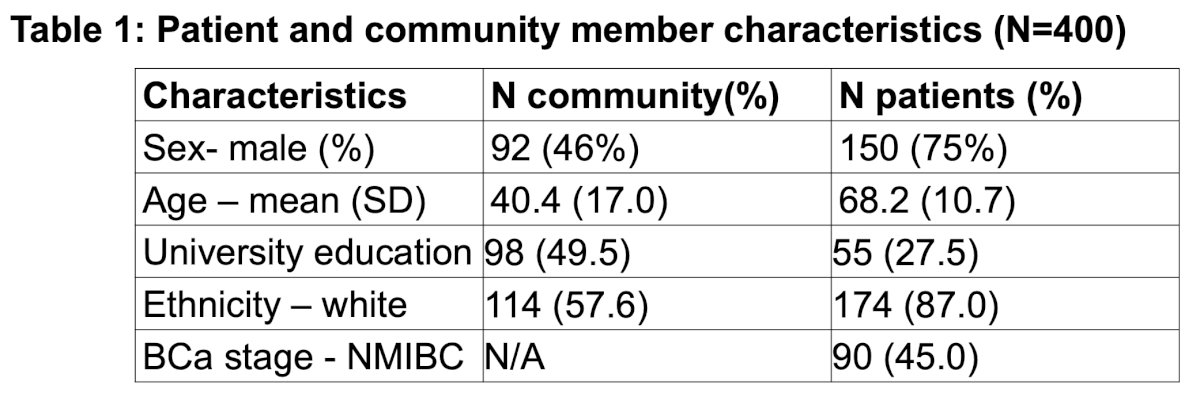
Of 400 participants, 322 completed the time tradeoff exercises with adequate comprehension:
Of the bladder cancer patients, 90 were non-muscle invasive bladder cancer, 53 muscle invasive bladder cancer and 32 had metastatic disease. A total of 3,288 randomly generated, unique BUSS-P health state valuations were obtained:
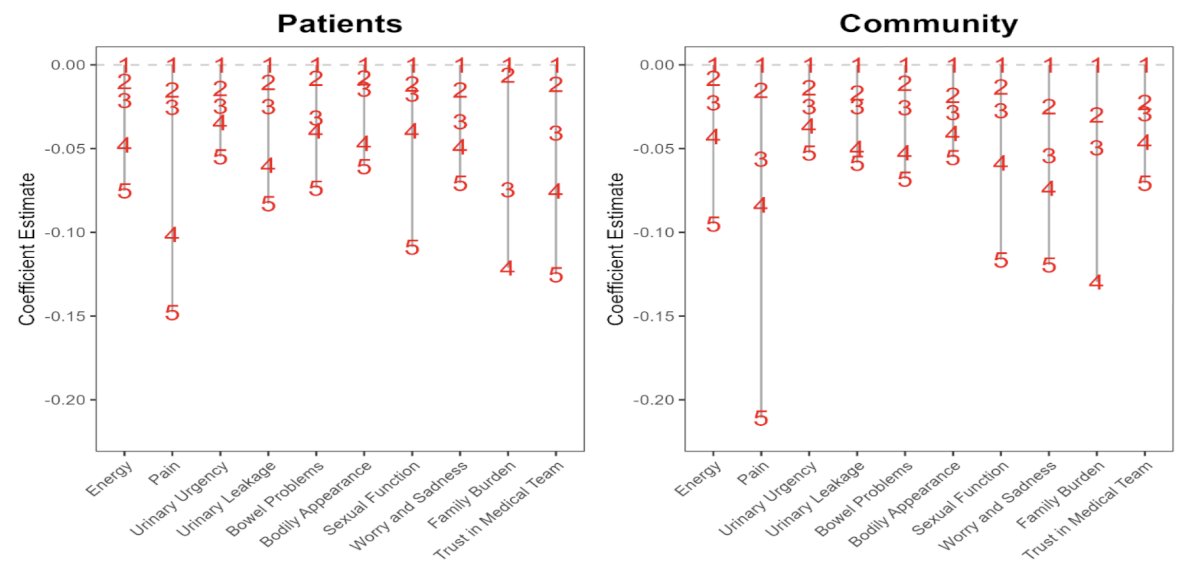
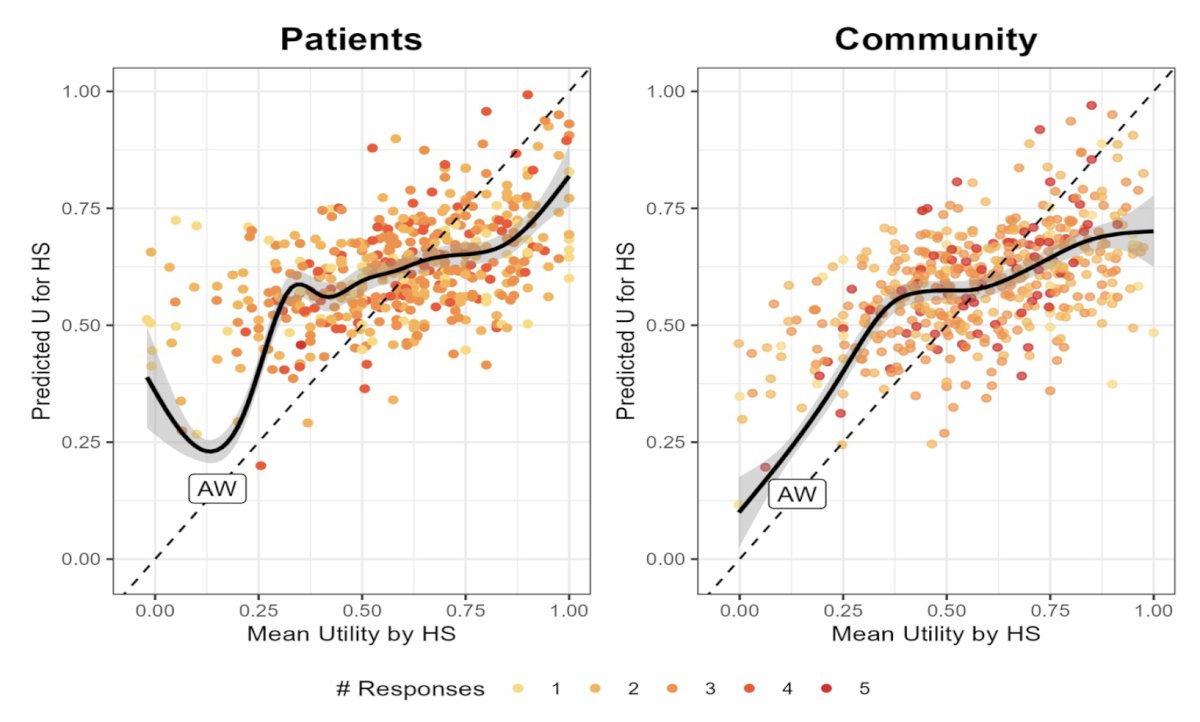
The predicted utility score can be estimated as 1 + the corresponding coefficient for each health state. An example using patient level weights is an individual with energy = 3, pain = 4, urinary urgency = 2, urinary leakage = 1, bowel problems = 2, bodily appearance = 5, sexual function = 3, worry and sadness = 4, family burden = 2, and trust in the medical team = 1, will have a predicted health utility of 1 – 0.021 – 0.101 – 0.014 + 0 – 0.008 – 0.061 – 0.017 – 0.049 – 0.006 = 0.793. Predictions were obtained from the final Bayesian linear regression model. The final model had a weighted correlation coefficient between predicted and observed utilities of 0.733 and 0.734 in the community and patient groups, respectively:
In an exploratory analysis of patients’ own BUSS-P responses, discrimination of utilities across health states was observed with mean utilities in non-muscle invasive bladder cancer, cystectomy, and minimally symptomatic metastatic patients at 0.897 (SD 0.099), 0.831 (SD 0.109) and 0.825 (SD 0.157), respectively.
Dr. Kulkarni concluded his presentation discussing the BUSS tool with the following conclusions:
- The BUSS-P is a simple 10-item questionnaire for which the investigators created two algorithms to calculate utilities for bladder cancer patients from its responses
- This is the first instrument that provides utilities for bladder cancer derived from both bladder cancer patients and the general public
- Grounded in robust time tradeoff methodology, utilities in all phases of bladder cancer care can be measured for use in comparative effectiveness research, cost-effectiveness, decision modeling, and policy work
Presented by: Girish Kulkarni, MD, PhD, FRCPC, University of Toronto, Princess Margaret Cancer Centre, Toronto, Canada
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th – April 8th, 2024