(UroToday.com) The 2024 European Association of Urology (EAU) annual congress held in Paris, France was host to a non-muscle invasive bladder cancer (NMIBC) abstract session. Dr. Hailong Hu presented the results of a prospective, comparative, within-patient multicenter phase III trial comparing blue light to white light cystoscopy for the detection of bladder cancer using modern high-definition 4K equipment.
Blue light cystoscopy (BLC) with hexaminolevulinate (HAL), a metabolic marker with tumor specificity/uptake, has proven efficacy for improving detection rates and subsequently reducing recurrence rates of bladder cancer, compared to white light cystoscopy (WLC). To date, no randomized controlled trials have been conducted using modern 4K LED equipment. System blue (Richard Wolf GmbH) is characterized by using a selected LED and an optimized illumination path for BLC, enabling System blue to exclusively exploit the autofluorescence of healthy tissue as background image for BLC. This sophisticated image detection, together with refined image processing, results in a unique differentiation between pathological and healthy tissue. The objective of this study was thus to compare HAL BLC with WLC for the detection of bladder cancer using novel equipment.
Patients with known or suspected bladder cancer were enrolled at one of seven hospitals, received intravesical HAL (Hexvix, Photocure ASA), and underwent both WLC and BLC (System blue, Richard Wolf GmbH; Figure 1).
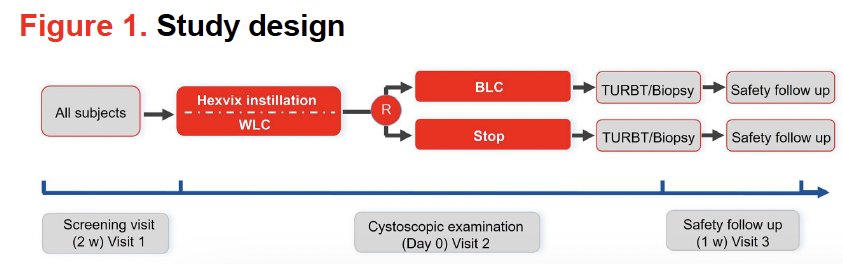
Lesions identified on WLC and BLC were recorded separately and evaluated by a blinded panel. The primary endpoint was the proportion of patients with NMIBC who had at least one such lesion found by HAL BLC, but not by WLC. Secondary endpoints included detection of carcinoma in situ, lesion detection rates, and device performance.
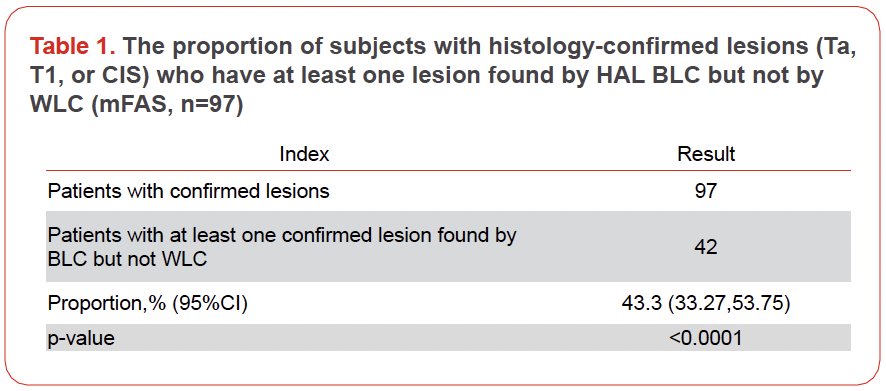
This trial included 158 patients, of whom 114 were included in the full analytic set. Of the 97 patients with Ta, T1, or CIS, 42 (43.3%) had ≥1 lesion found by BLC, but not by WLC (p<0.001).
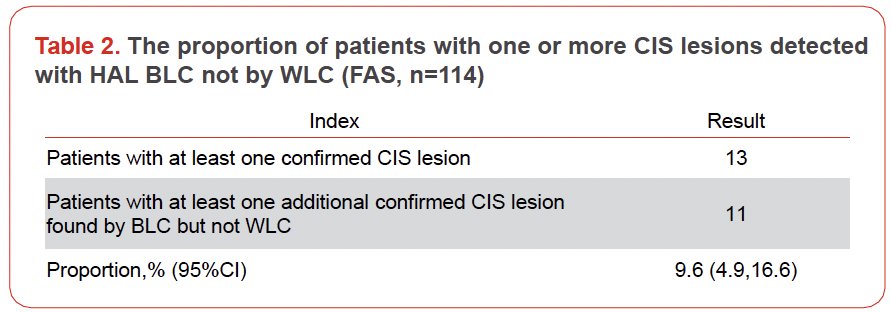
Of the 114 patients, 13 (11.4%) had CIS. Of these 13 patients, 11 (85%) had additional CIS lesions only detected with BLC, but not WLC.
Summarized in the table below is the lesion detection rate for HAL BLC and WLC for PUNLMP, CIS, Ta, T1, T2-4 and the proportion of false positive lesions detected with HAL BLC and WLC:
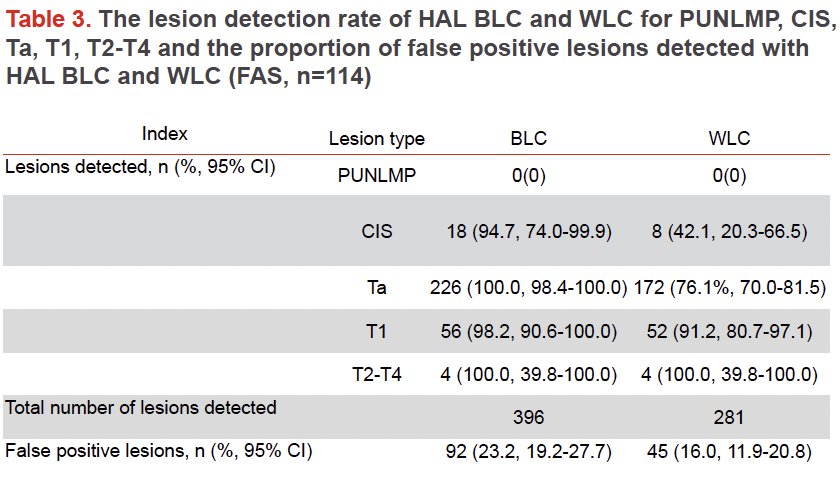
Physicians rated image quality in BLC mode as excellent in 89% of cases and good in the remaining 11%. The overall satisfaction with device performance was reported as excellent and good by 84% and 12% of operators, respectively.
Dr. Hu concluded as follows:
- This study confirms the superiority of HAL BLC over WLC for the detection of bladder cancer even if improved WLC modalities using HD 4K equipment are utilized.
- In particular, additional high-risk, difficult-to-see CIS lesions have been identified in 85% of all CIS patients only by HAL BLC.
- The quality of resection is still a key cornerstone in the treatment of NMIBC of which BLC remains a crucial part, despite the further development of WLC imaging.
Presented by: Hailong Hu, Peking Union Medical College Hospital, Department of Urology, Beijing, China
Written by: Rashid Sayyid, MD, MSc – Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th – April 8th, 2024


