(UroToday.com) The 2024 European Association of Urology (EAU) annual meeting featured a meeting of the EAU Section of Oncologic Urology (ESOU) and the European Urology Oncology lecture by Dr. Alicia Morgans discussing survivorship considerations across the spectrum of genitourinary oncology. Dr. Morgans started her presentation by highlighting that cancer survivorship begins at diagnosis and through the balance of an individual’s life. Genitourinary cancer survivors also include those living with cancer and those free of cancer:

Notably, there is a difference between survivorship versus palliative care and symptom management. Survivorship care focuses on longitudinal services that allow optimal treatment and follow-up over time. One important consideration is cardio-oncology care, which enables ongoing cancer-directed therapy and long-term monitoring for secondary malignancies after radiation. Contrarily, palliative care and symptom management focus on relieving bothersome symptoms and are time limited:

Dr. Morgans highlighted that the cancer survivor population is increasing, with nearly 26.1 million cancer survivors expected by 2040:

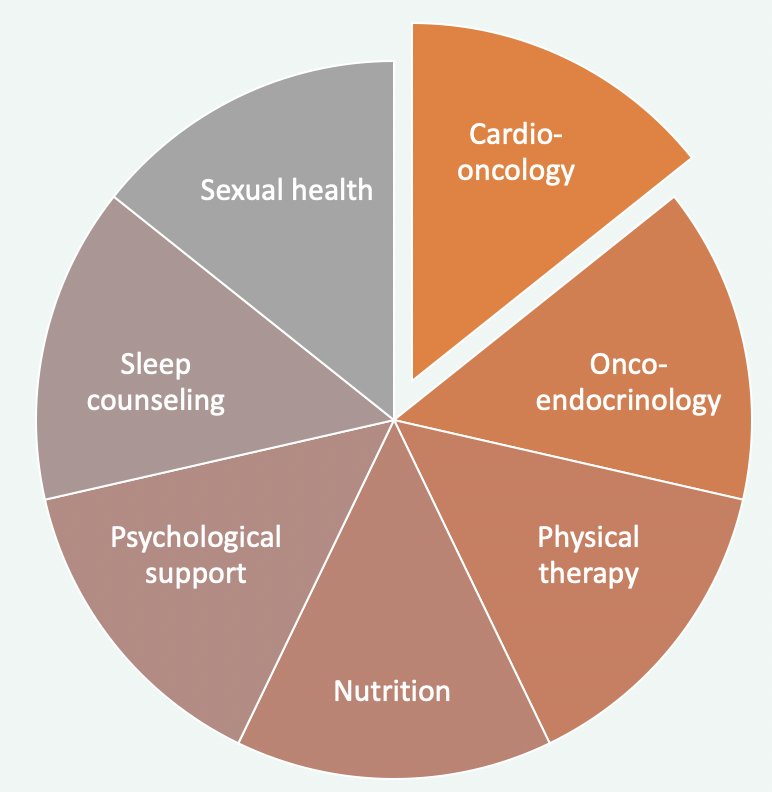
The Commission on Cancer in the United States put forth new standards for care in 2020, and survivorship programs should strive to support the whole patient with comprehensive services across many disciplines:
As such, the key areas of cancer survivorship according to Dr. Morgans include:
- Prevention of cancer recurrence and new cancer
- Long term side effects of cancer or treatment
- Addressing modifiable health behaviors
- Ensuring care coordination
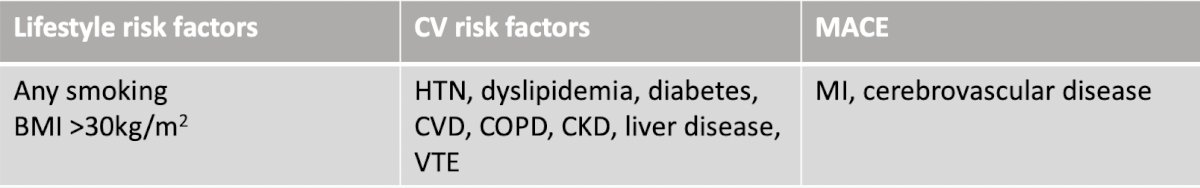
Looking at specific aspects of survivorship, Dr. Morgans started with cardiovascular disease, which is the most common cause of death in European men. Indeed, cardiovascular risk factors are affected by ADT: (i) increased total cholesterol, (ii) increased triglycerides, (iii) increased abdominal adipose tissue, (iv) impaired glucose metabolism, and (v) weight gain. Cardiovascular risk factors are present in 92.5% of patients receiving androgen deprivation therapy. Additional risk factors are as follows:
With regards to testicular cancer patients, treatment of testicular cancer is associated with increased risk of dyslipidemia, hypertension, insulin resistance, and weight gain. Metabolic syndrome affects up to 25% of testicular cancer survivors after platinum-based chemotherapy and risk factors identified with higher rates of cardiovascular disease and cardiovascular events include1:
- Cisplatin combination chemotherapy: HR 1.9, 95% CI 1.1-3.1 versus orchiectomy
- Obesity at diagnosis: HR 4.6, 95% CI 2.0-10.0 versus normal BMI
- Smoking at diagnosis: HR 1.7, 95% CI 1.1-2.4 versus non-smoking
- Developed Raynaud’s phenomenon: HR 1.9, 95% CI 1.1-36 versus those that did not
- Developed dyslipidemia: HR 2.8, 95% CI 1.6-4.7 versus those that did not
- Positive family history: HR 2.9, 95% CI 1.7-4.9 versus those without
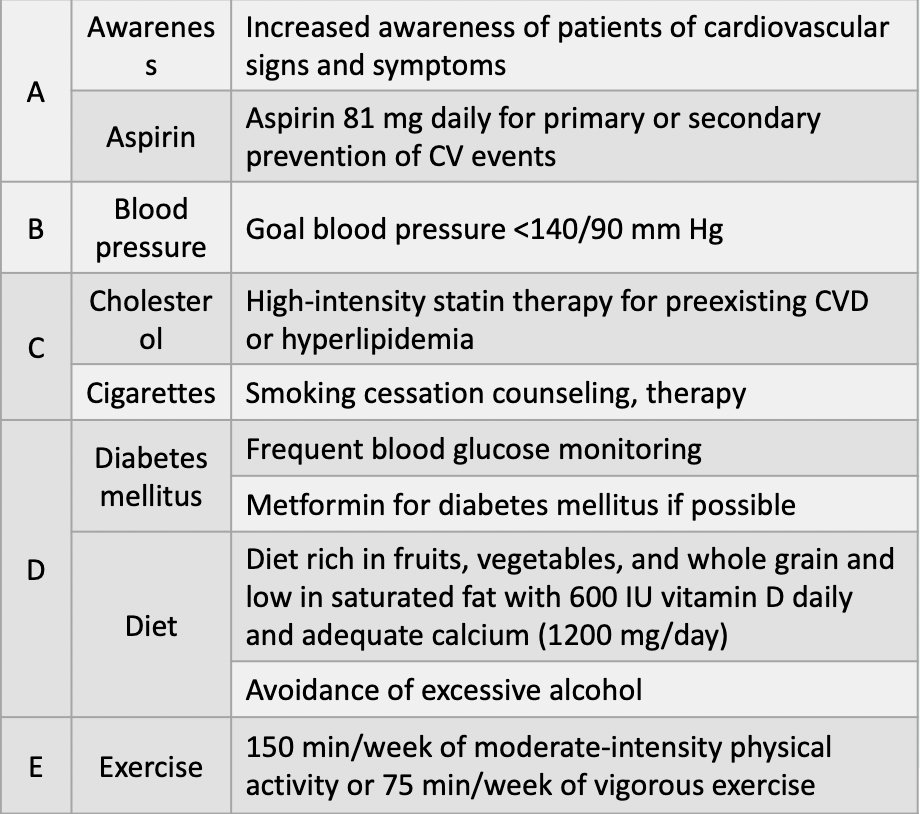
The 2023 NCCN Guidelines suggest assessing traditional risk factors for cardiovascular disease, including a team approach, specifically partnering management of patients with a primary care team, and counseling survivors on any increased risk of cardiovascular disease based on prior treatment. High risk patients may need to be followed by a cardiologist in addition to the oncology/urology teams. The following figure is provided by the NCCN:
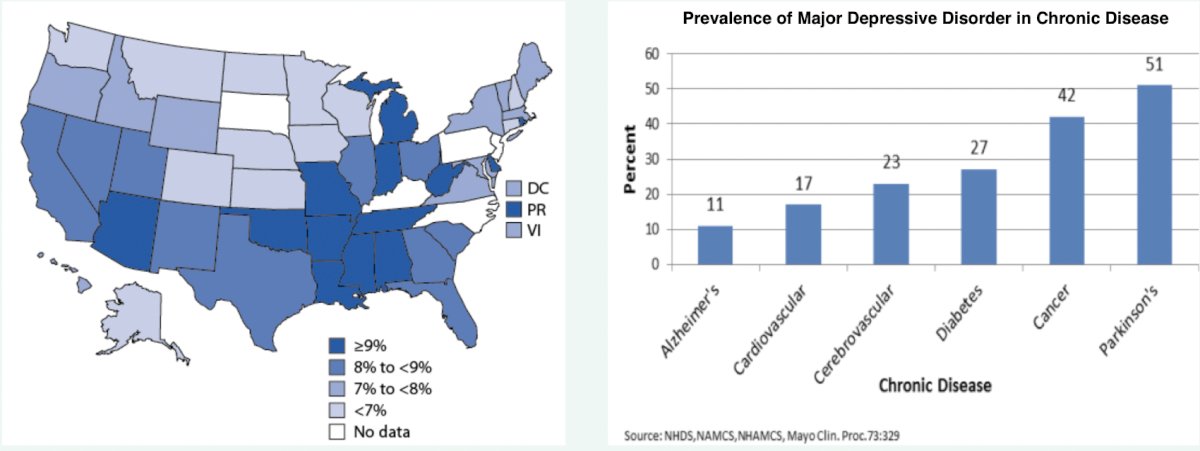
With regards to mental health, Dr. Morgans notes that the impact of depression in the United States is vast, with cancer patients making up the second most likely group to be depressed (42%) after only those with Parkinson’s disease:
There is also increasing evidence that ADT for locally advanced and metastatic PCa is associated with depression. A study from 2016 using SEER-Medicare data found that men that received ADT, compared with patients who did not receive ADT, had higher 3-year cumulative incidences of depression (7.1% v 5.2), inpatient psychiatric treatment (2.8% v 1.9%), and outpatient psychiatric treatment (3.4% v 2.5%).2 Furthermore, the risk of depression increased with duration of ADT, from 12% with ≤ 6 months of treatment, 26% with 7 to 11 months of treatment, to 37% with ≥ 12 months of treatment.
For patients with muscle invasive bladder, using the SEER-Medicare database from 2002 to 2011, Jazzar and colleagues3 identified 3,709 patients who were diagnosed with clinical stage T2 through T4a bladder cancer of which 1,870 (50.4%) were diagnosed with posttreatment psychiatric disorders. Patients who underwent radical cystectomy were identified as being at significantly greater risk of having a posttreatment psychiatric illness compared with those who received radiotherapy and/or chemotherapy (HR 1.19, 95% CI 1.07-1.31):
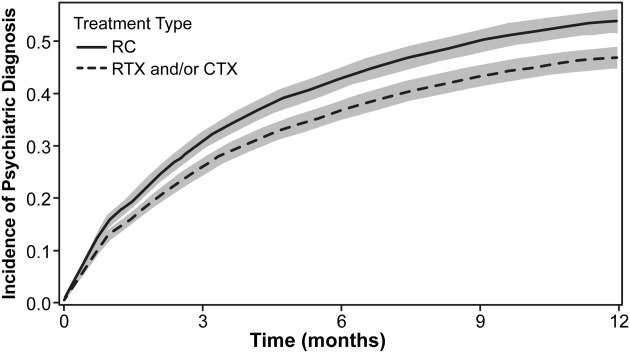
Furthermore, in adjusted analyses, diagnosis of a psychiatric disorder resulted in significantly worse overall survival (HR 2.80, 95% CI, 2.47-3.17) and cancer-specific survival (HR 2.39, 95% CI, 2.05-2.78).
A 2021 population-level study published in the Journal of Clinical Oncology evaluated the impact of a testicular cancer diagnosis and treatment on subsequent mental illness and utilization of mental illness healthcare resources.4 This study included all incident cases of testicular cancer treated with orchiectomy in Ontario, Canada from 2000 to 2010, identified using the Ontario Cancer Registry. Cases were matched to controls in a 1:5 ratio based on age and geography. Additional population-level databases were used to identify mental health service use episodes, which included outpatient use accounting for visits to a general practitioner for a mental health concern or any visit to a psychiatrist. The authors used negative binomial regression modeling to estimate the rate of mental health service use in the pretreatment (2 years prior until 1 month before orchiectomy), peri-treatment (1 month before until 1 month after orchiectomy), and post-treatment periods (1 month after orchiectomy until end of follow-up). Overall, there were 2,619 cases of testicular cancer matched to 13,095 controls, for which there was no baseline difference in the rate of mental health service use. Patients with testicular cancer were significantly more likely than controls to have an outpatient visit for a mental health concern in the peri-treatment (adjusted rate ratio [aRR] 2.45, 95% CI 2.06 to 2.92) and post-treatment periods (adjusted RR 1.30, 95% CI 1.12 to 1.52). The difference in mental health service use persisted over a median follow-up of 12 years:
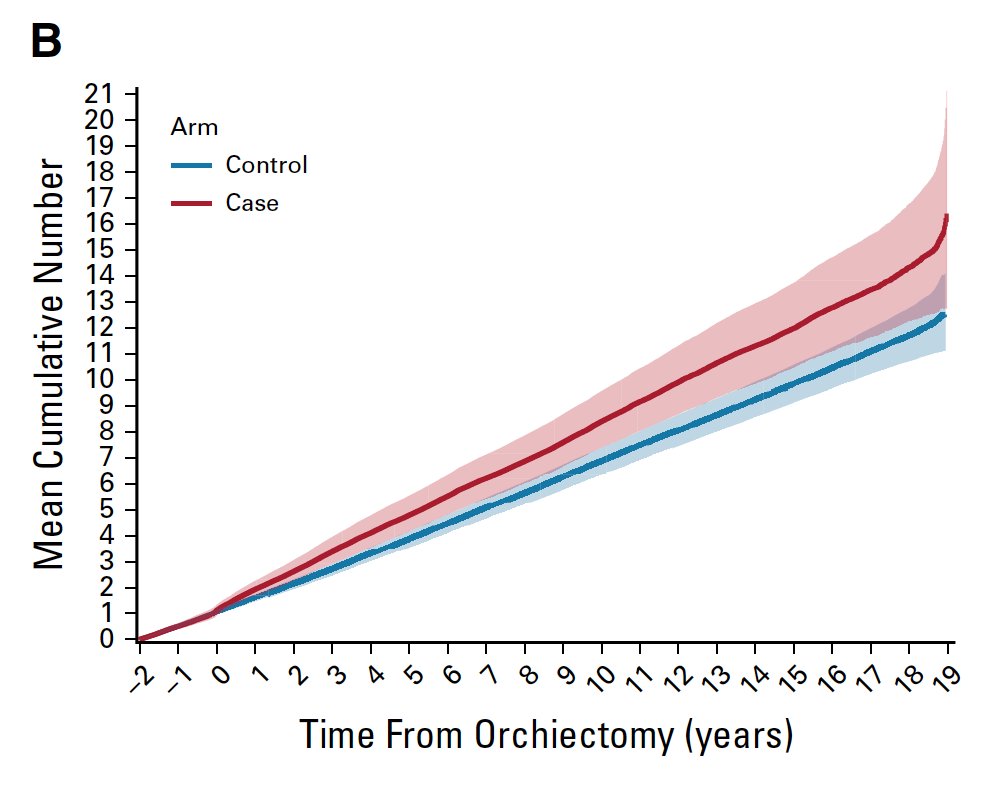
In the post-orchiectomy period, cases with baseline mental health service use were those most likely to use mental health services (adjusted RR 5.64, 95% CI, 4.64 to 6.85). Furthermore, In
the pre-treatment period, cases and controls had comparable use of mental health services for anxiety (61% v 51%) and depression (11% v 7%); controls had substantially more visits for substance-related and addictive disorders (33% v 18%).
The NCCN guidelines for survivorship state that general screening recommendations are available for depression and for the impact of mood symptoms on functioning. Additionally, effective treatments for depression should be considered, including exercise, counseling, and pharmacologic strategies.
Finally, Dr. Morgans discussed sexual health and the effect of treatment for genitourinary cancers. Previous studies assessing treatment for genitourinary cancers and subsequent risk of erectile dysfunction suggest that erectile dysfunction is often associated with orchiectomy, upper tract and lower urinary tract urothelial carcinoma, renal cancer, and penile cancer, in addition to the well-established relationship with prostate cancer.
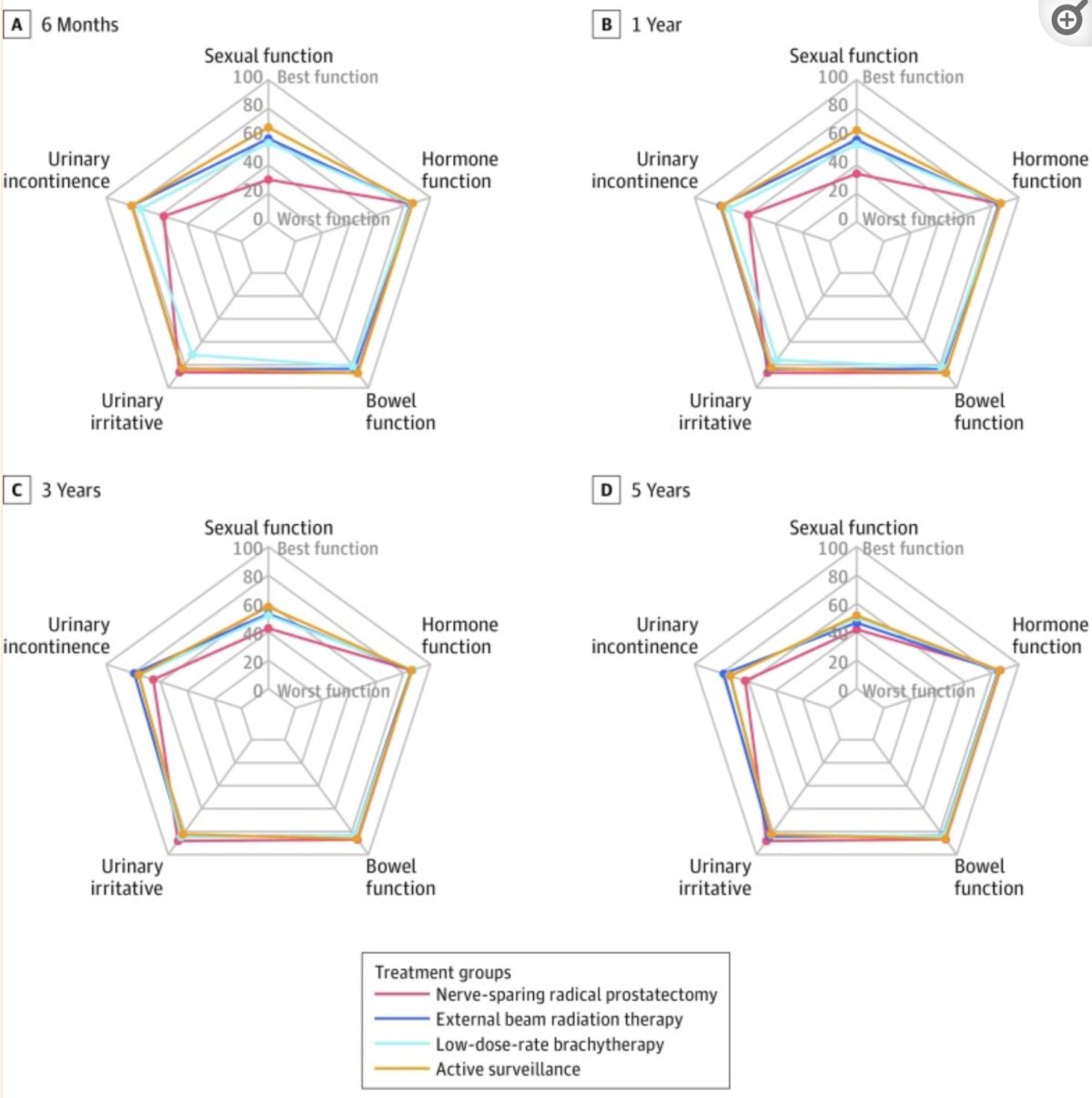
Work from the CEASAR cohort5 assessed 2,005 patients with intermediate risk localized prostate cancer, comparing sexual health and other quality of life outcomes by treatment. Prostatectomy was associated with poorer sexual function at 6 months, and radiation with ADT was superior at 5 years post-diagnosis for unfavorable intermediate patients:
For bladder cancer patients, there have been 37 studies focusing on sexual health, including 15 on men, 10 focused on women, and 11 assessing both. Most of these studies focused on muscle invasive bladder cancer, with a lack of standardized measures to assess aspects of sexual health (function, interest, etc) for all patients. Differences are documented between clinician views of importance of sexual health when compared to those of patients. Moreover, >= 50% of women reported never having been counseled about the importance of sexual health, despite radical cystectomy routinely involving vaginal resection.
Dr. Morgans emphasized that it is important to determine which causes of sexual dysfunction are at play, noting that identifying the cause(s) can help find solutions:
- Erectile dysfunction: post-surgical or radiation due to hormonal therapy, medications, comorbidities, aging, etc
- Vaginal dryness: atrophy, dysfunction post-surgery or radiation
- Loss of libido: secondary to hormonal changes, psychological
- Psychological distress due to cancer and/or treatment
- Body dysmorphia
- Many others
Ultimately, there are many opportunities for multidisciplinary approaches that may help to medically optimize patients receiving treatment:

As new therapies arise in genitourinary oncology, this raises the opportunity for involving new teams to address potential novel long-term toxicities. Additionally, adjuvant and maintenance treatment regimens result in patients living longer on therapy than they have previously.
Dr. Morgans concluded her presentation by discussing survivorship considerations across the spectrum of genitourinary oncology with the following conclusions:
- Cancer survivors are anyone living with or beyond a diagnosis of cancer
- Complications including cardiovascular, psychological, and sexual health concerns are some of the most prevalent concerns across all genitourinary cancers
- A standardized approach to implementing survivorship care can reduce suffering, enhance well-being, and improve the lives of patients
- Supporting cancer survivorship clinicians and programs to innovate in terms of support services, research, and education is critical
Presented by: Alicia K. Morgans, MD, MPH, Dana Farber Cancer Institute, Boston, MA
Written by: Zachary Klaassen, MD, MSc – Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, Wellstar MCG Health, @zklaassen_md on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th – April 8th, 2024
References:
- Lubberts S, Groot HJ, de Wit R, et al. Cardiovascular Disease in Testicular Cancer Survivors: Identification of Risk Factors and Impact on Quality of Life. J Clin Oncol. 2023 Jul 1;41(19):3512-3522.
- Dinh KT, Reznor G, Muralidhar V, et al. Association of Androgen Deprivation Therapy With Depression in Localized Prostate Cancer. J Clin Oncol. 2016;34(16):1905-1912.
- Jazzar U, Yong S, Klaassen Z, et al. Impact of psychiatric illness on decreased survival in elderly patients with bladder cancer in the United States. Cancer 2018; 124(15): 3127-35.
- Raphael MJ, Gupta S, Wei X, et al. Long-Term Mental Health Service Utilization Among Survivors of Testicular Cancer: A Population-Based Cohort Study. J Clin Oncol. 2021;39(7):779-786.
- Hoffman KE, Penson DF, Zhao Z, et al. Patient-Reported Outcomes Through 5 Years of Active Surveillance, Surgery, Brachytherapy, or External Beam Radiation with or without Androgen Deprivation Therapy for Localized Prostate Cancer. JAMA 2020 Jan 14;323(2):149-163.


