(UroToday.com) The 2024 European Association of Urology (EAU) annual meeting featured a plenary session highlighting risk adapted screening for prostate cancer in Europe and a presentation by Dr. Alicia Morgans discussing familial prostate cancer and whether it influences screening and management. Dr. Morgans started by highlighting the EAU guideline’s position on germline testing:
- Consider germline testing in men with metastatic prostate cancer (strength rating: weak)
- Consider germline testing in men with high-risk prostate cancer who have a family member diagnosed with prostate cancer at age < 60 years (strength rating: weak)
- Consider germline testing in men with multiple family members diagnosed with prostate cancer at age < 60 years or a family member who died from prostate cancer (strength rating: weak)
- Consider germline testing in men with a family history of high-risk germline mutations or a weak family history of multiple cancers on the same side of the family (strength rating: weak)
Dr. Morgans notes that this appropriately broad approach to genetic testing will identify many people without prostate cancer with BRCA2 mutations. With regards to the EAU guideline’s stance on screening and individual early detection:
- Offer early PSA testing to well-informed men at elevated risk of having prostate cancer (strength rating: strong):
- Men from 50 years of age
- Men from 45 years of age and a family history of prostate cancer
- Men of African descent from 45 years of age
- Men carrying BRCA2 mutations from 40 years of age
Importantly, work from the initial screening round of the IMPACT study showed that among patients with BRCA2 mutations, the PPV of screening for prostate cancer at a PSA >=3 ng/mL was 48% versus 33% for non-carriers.1 Follow-up results from this study showed that patients with BRCA2 mutations were diagnosed at a younger age (61 versus 64 years, p = 0.044), and were more likely to have intermediate or high-risk disease (p = 0.011).2
Although there has been much attention in the metastatic prostate cancer setting for DNA repair gene mutations, this has not been as thoroughly studied in the localized setting until recently. Lee et al. performed a single institution cross sectional study assessing mutations in 1,588 patients with localized prostate cancer, noting a mutation rate of 4% in European ancestry patients.3 Among these patients, 21% had high risk disease, including 3.7% with a germline mutation, and 1% with a BRCA2 mutation. Furthermore, 11% of patients had very-high risk disease, including 6.2% of very high risk men with a germline mutation having a BRCA2 mutation: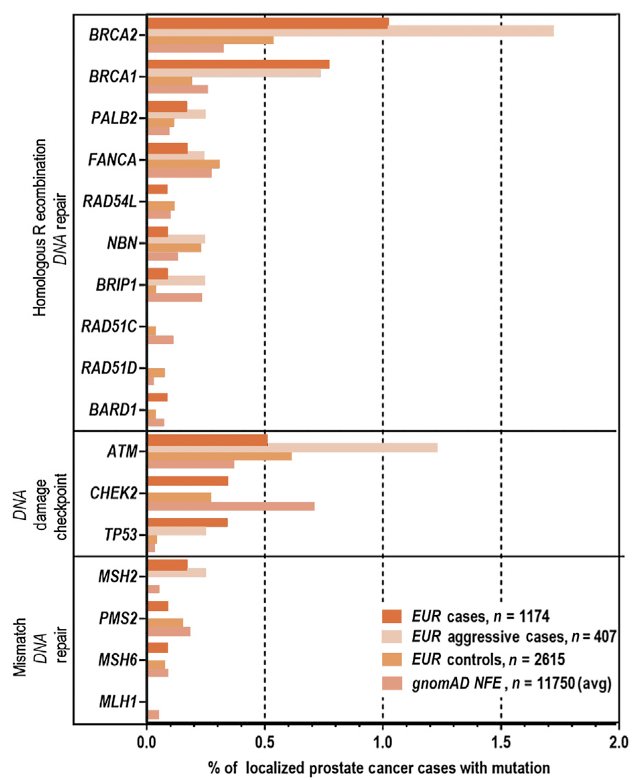
With regards to the impact on treatment, Carter et al. assessed the impact of germline mutations in ATM and BRCA1/2 on grade reclassification in men on active surveillance.4 Among two US institutional cohorts, there were 1,211 patients with localized prostate cancer of which 289 underwent grade reclassification. Furthermore, reclassification occurred in 6 of 11 BRCA2 mutation carriers versus 283 of 1,200 non-carriers (aHR 2.74, 95% CI 1.26-5.96), and BRCA2 patients were more likely to have Gleason score upgrade: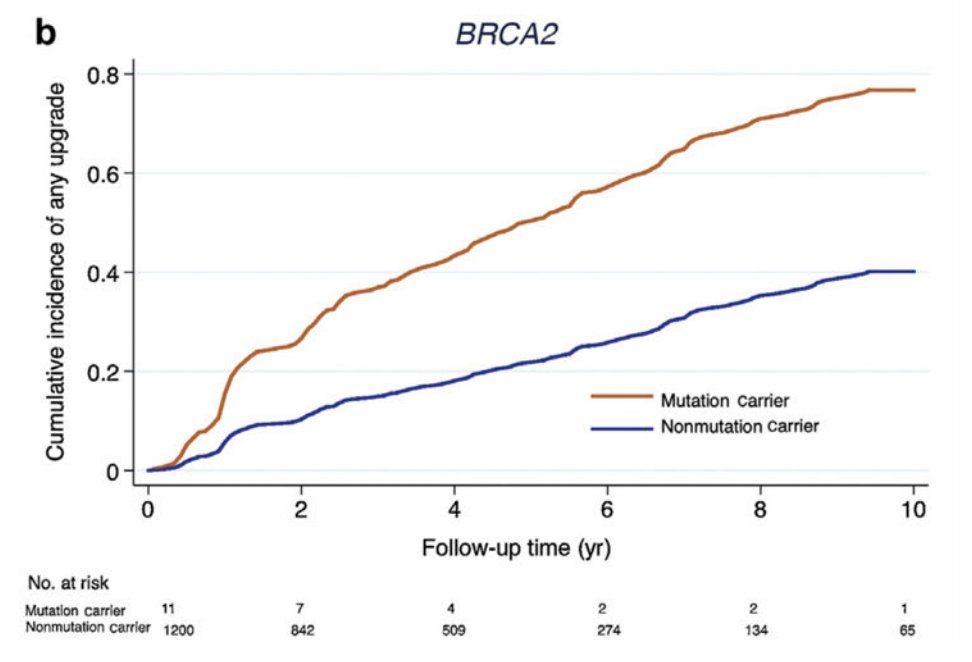
Castro et al. previously assessed the effect of BRCA mutations on metastatic relapse and cause-specific survival after radical treatment among 1,302 patients with localized or locally advanced prostate cancer.5 In this study, 67 patients had BRCA2 mutations and 1,235 were non-carriers, with more high-risk carriers treated with radiation (68.8% versus 34.4%). Additionally, patients with BRCA2 mutations had poorer outcomes in metastasis free survival and cancer specific survival with definitive treatment: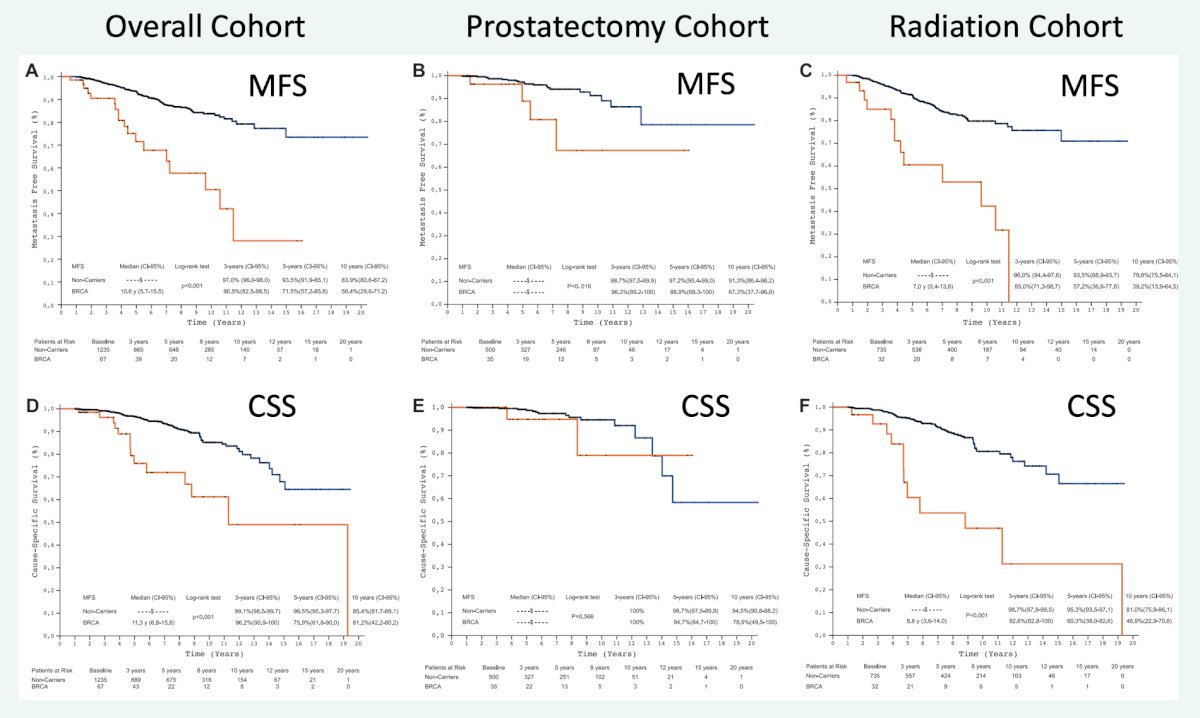
Dr. Morgans noted that there are additional important aspects from the NCCN specific to those with BRCA-pathogenic/likely pathogenic variant positive management. For male breast cancer screening, these men are encouraged to undergo an annual mammogram given the 7% lifetime risk of breast cancer. For pancreatic cancer screening, the panel does not currently recommend screening for carriers in genes other than STK11 and CDKN2A in the absence of a close family history of exocrine pancreatic cancer.
For implementing screening recommendations, Dr. Morgans discussed the ProGen multisite randomized controlled trial, which included 662 participants with high risk localized or metastatic prostate cancer from 3 institutions. Patients were randomly assigned to the video education or genetic counselor arms, with similar knowledge of their disease between the groups. Among the patients with pathologic variant mutations, there was slightly lower distress with genetic counseling and a slightly higher positive experience with video education: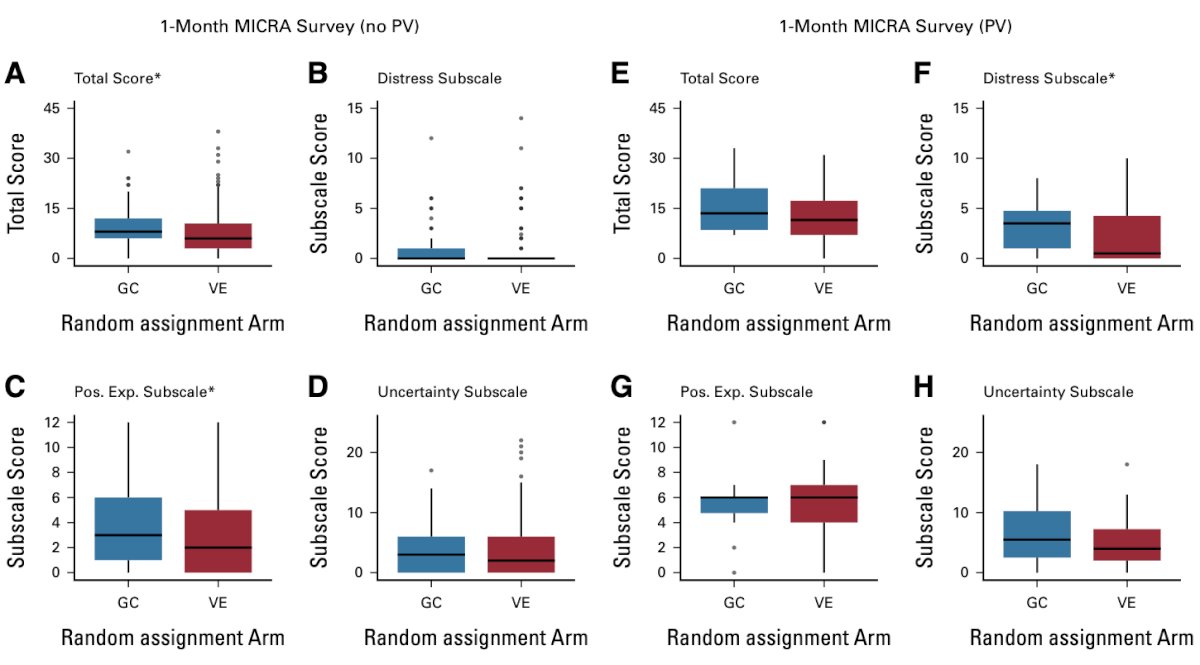
Dr. Morgans concluded her presentation discussing familial prostate cancer and whether it influences screening and management with the following conclusions:
- The EAU guidelines (and others) recommend germline testing for metastatic patients and localized patients with a family history, thus identifying patients with BRCA mutations without cancer may become more common
- BRCA mutation patients are more likely to have upstaging during follow-up with active surveillance
- Screening for male breast cancer with self exams +/- mammograms at 35 is recommended
- Screening for pancreatic cancer can be considered with a family history
- Implementing widespread testing will require scalable solutions
Presented by: Alicia Morgans, MD, MPH, Genitourinary Medical Oncologist, Medical Director of Survivorship Program at Dana-Farber Cancer Institute, Boston, Massachusetts
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, WellStar MCG Health, @zklaassen_md on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th - April 8th, 2024
References:
- Bancroft EK, Page EC, Castro E, et al. Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: Results from the initial screening round of the IMPACT study. Eur Urol. 2014 Sep;66(3):489-499.
- Page EC, Bancroft EK, Brook MN, et al. Interim results from the IMPACT study: Evidence for Prostate-specific Antigen screening in BRCA2 mutation carriers. Eur Urol. 2019 Dec;76(6):831-842.
- Lee DJ, Hausler R, Le AN, et al. Association of inherited mutations in DNA repair genes with localized prostate cancer. Eur Urol. 2022 Jun;81(6):559-567.
- Carter HB, Helfand B, Mamawala M, et al. Germline mutations in ATM and BRCA1/2 are associated with grade reclassification in men on active surveillance for prostate cancer. Eur Urol. 2019 May;75(5):743-749.
- Castro E, Goh C, Leongamornlert D, et al. Effect of BRCA Mutations on Metastatic Relapse and Cause-Specific Survival after Radical Treatment for Localized Prostate Cancer. Eur Urol. 2015 Aug;68(2):186-193.
- Rana HQ, Stopfer JE, Weitz M, et al. Pretest video education versus genetic counseling for patients with prostate cancer: ProGen, A multisite randomized controlled trial. JCO Oncol Pract. 2023 Nov;19(11):1069-1079.


