(UroToday.com) The 2024 European Association of Urology (EAU) annual meeting featured a plenary session on personalized approaches in high-risk and metastatic prostate cancer, and a state of the art lecture by Dr. Roderick Van Den Bergh discussing clinical and molecular stratification of men with biochemical recurrence after radical prostatectomy. Dr. Van Den Bergh notes that biochemical recurrence is a very heterogeneous disease space:
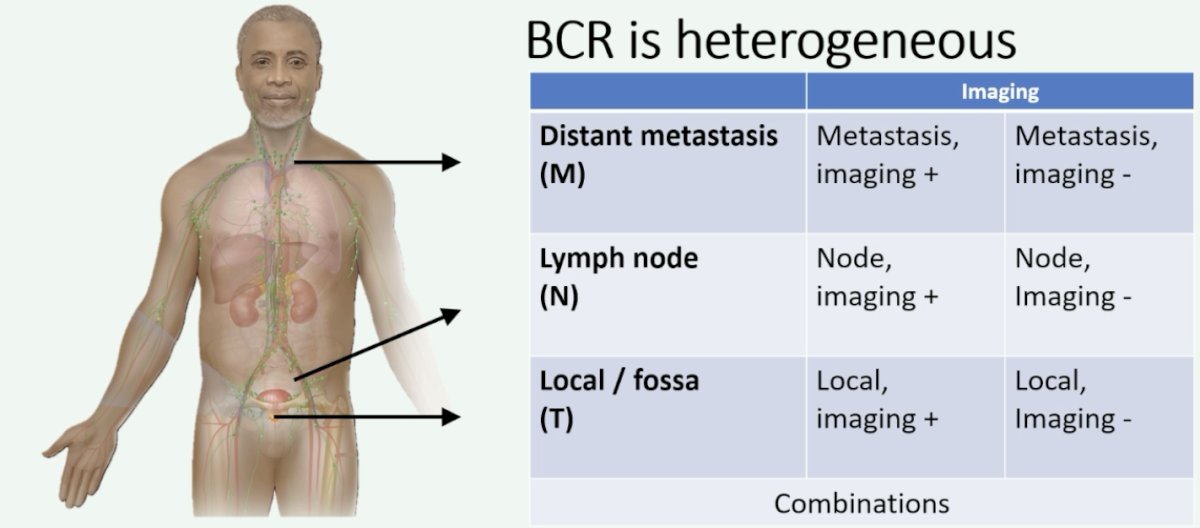
There are several potential treatment options for these patients, including:
- Watchful waiting
- Salvage radiotherapy to the prostatic fossa (+ ADT?)
- Salvage radiotherapy to the pelvis (+ ADT?)
- Oligo-/stereotactic therapy (+ ADT?)
- ADT (with intensification?)
The aims of biochemical recurrence management include (i) selecting the right therapy for the right patient, (ii) avoiding overtreatment and under-treatment, (iii) improving long-term oncological endpoints, and (iv) minimizing side effects of salvage therapy. But, having said this, Dr. Van Den Bergh emphasizes that it is of the utmost importance to use common sense on a patient by patient basis.
The iceberg we can see above the water is often a patient receiving early salvage radiotherapy to the fossa for a PSA < 0.5 ng/mL. However, beneath the surface are important factors:
- Patient factors: age, comorbidity, life expectancy
- Risk stratification: heterogeneous disease spectrum
- Imaging: PSMA PET, other predictors
- Alternative therapeutic options: stereotactic ablative radiotherapy, systemic intensification
Dr. Van Den Bergh provided the following treatment algorithm for biochemical recurrence, which he subsequently went through in detail for the remainder of his presentation: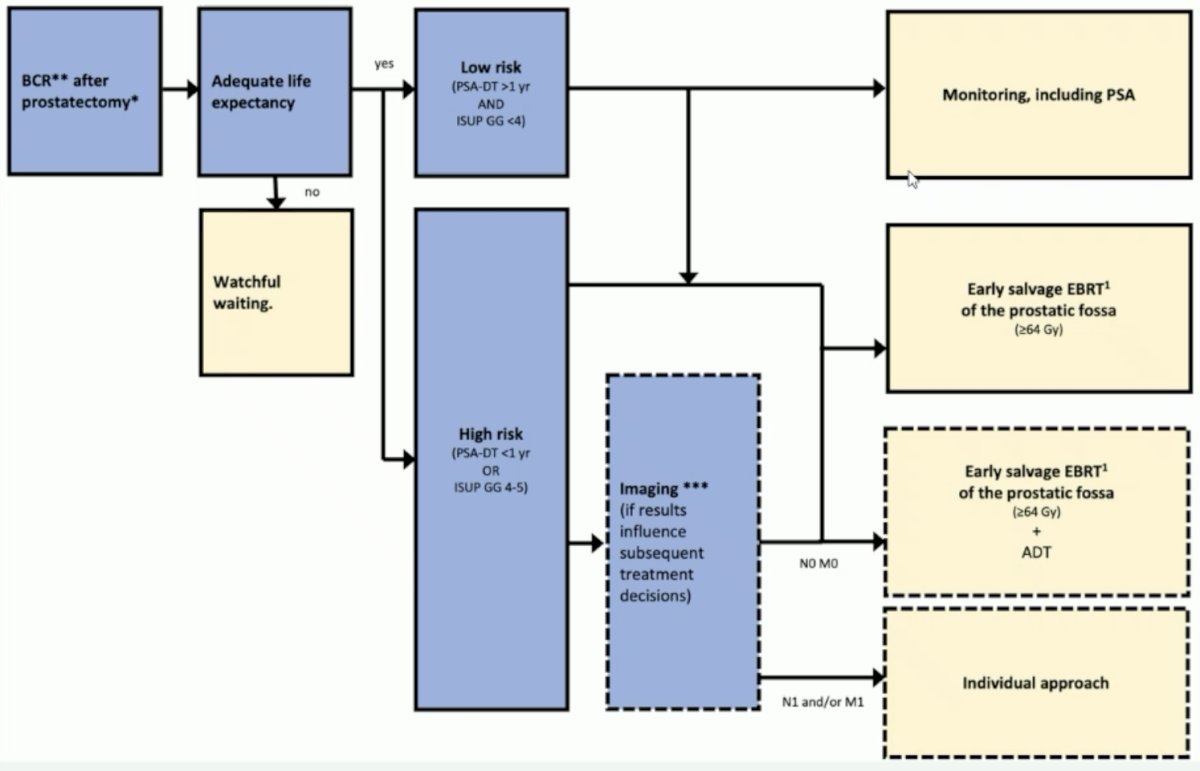
For patients who do not have an adequate life expectancy, watchful waiting is an appropriate surveillance plan. For these patients, it is important to weigh improved oncologic outcomes, side effects, and the natural history of the disease. For patients with an adequate life expectancy, triaging patients as low versus high risk is the next step in management. In 2019, the EAU published biochemical recurrence risk groups after radical prostatectomy, noting that low risk patients are those with a PSA doubling time > 12 months and pathologic Gleason Group 1-3. High risk patients are those with PSA doubling time < 12 months or pathologic Gleason Group 4-5. Recently, Preisser and colleagues validated the EAU biochemical recurrence risk groups via a multicenter approach.2 Among 2,379 patients at 10 centers, there were 805 and 1,574 patients were classified as having EAU low- and high-risk biochemical recurrence, respectively. For both overall survival (p < 0.0001) and cancer specific survival (p < 0.0001) low risk biochemical recurrence had improved outcomes versus high risk: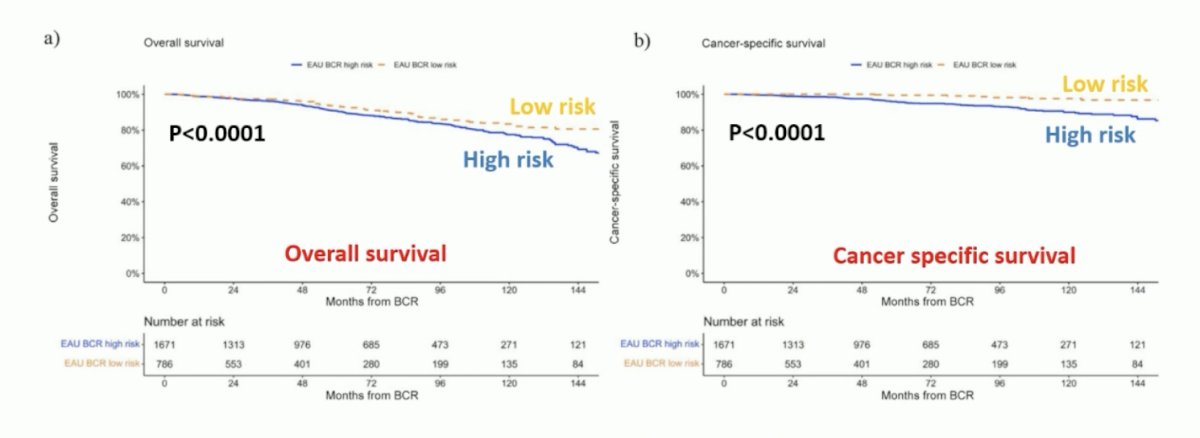
For low-risk biochemical recurrence, 12-year overall survival was 87% versus 78% (p = 0.2) and cancer-specific survival was 100% versus 96% (p = 0.2) for early versus no salvage radiotherapy. For high-risk biochemical recurrence, 12-year overall survival was 81% versus 66% (p < 0.001) and cancer-specific survival was 98% versus 82% (p < 0.001) for early versus no salvage radiotherapy: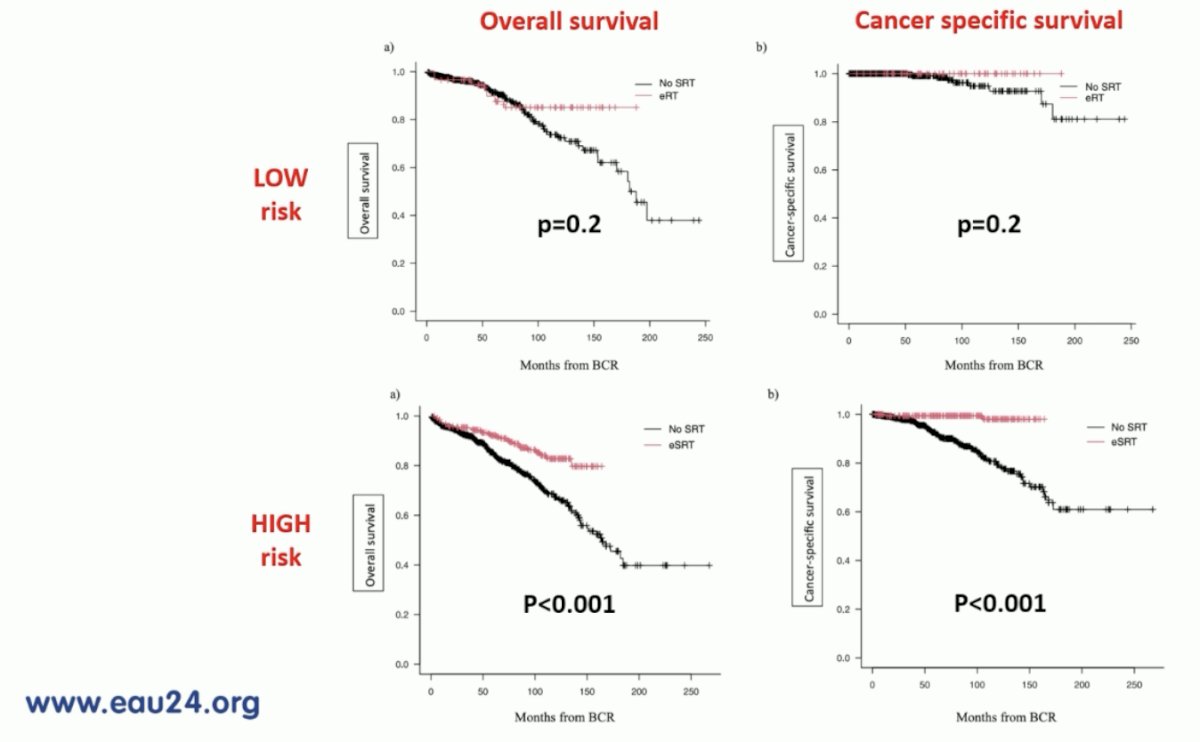
In multivariable analyses, early salvage radiotherapy decreased the risk of death (HR 0.55, p < 0.01) and cancer-specific death (HR 0.08, p < 0.001). Late salvage radiotherapy was a predictor of cancer-specific death (HR 0.17, p < 0.01) but not death (HR 0.66, p = 0.1).
For patients with high risk biochemical recurrence, Dr. Van Den Bergh discussed the importance of imaging. The following summarizes the EAU guidelines for PSA and PSMA PET positivity: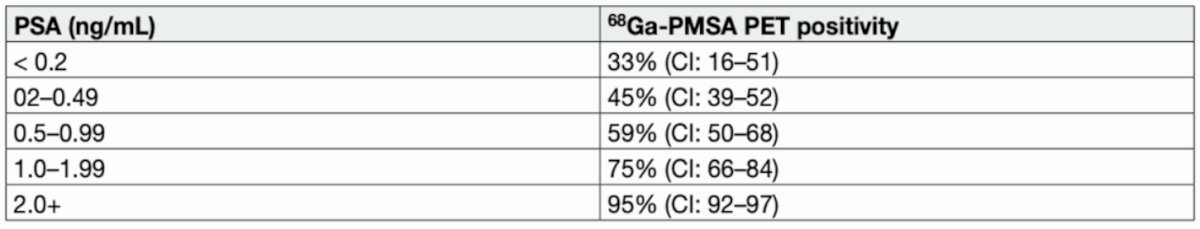
Recent studies have suggested that PSMA PET/CT filters biochemical recurrence cases. In 2020, Emmett and colleagues aimed to evaluate the predictive value of PSMA PET for a 3-year freedom from progression in men with biochemical recurrence after radical prostatectomy undergoing salvage radiotherapy.3 Among 260 men, the median PSA was 0.26 ng/mL (IQR 0.15-0.59 ng/mL), and follow-up was 38 months (IQR 31-43). PSMA PET had negative results in 34.6%, showed disease confined to the prostatic fossa in 21.5%, showed disease in the pelvic nodes in 26.2%, and showed distant disease in 17.7%. Among these patients, 71.5% received salvage radiotherapy. PSMA PET was highly predictive of freedom from progression at 3 years after salvage radiotherapy. Overall, freedom from progression was achieved in 64.5% of those who received salvage radiotherapy, 81% with negative results or fossa-confined findings versus 45% with extra-fossa disease (p < 0.0001). There were 32% of men with a negative PSMA PET who did not receive treatment, and among these, 66% progressed, with a mean rise in PSA of 1.59 ng/mL over the 3 years.
The final trial discussed was the PSMA-SRT trial, a randomized prospective phase III trial of 68Ga-PMSA-11 PET/CT salvage radiotherapy planning.4 In this trial, there were 193 patients enrolled from September 6, 2018, to August 17, 2020: 90 were randomized to the control group, and 103 were randomized to the PSMA group: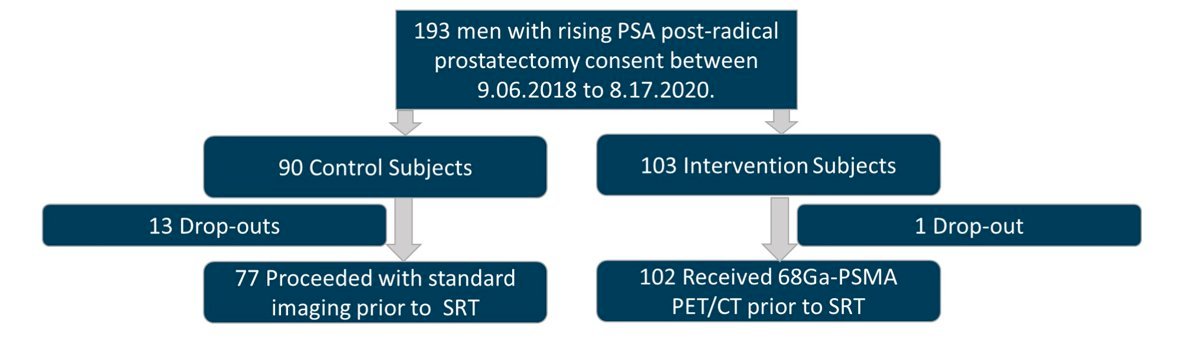
The median time from radical prostatectomy to enrollment and median PSA was 20.3 months (IQR 1.4–245) and 0.3 ng/ml (IQR 0.2-10.3) for the control group, and 28.3 months (IQR 1.2–21) and 0.23 ng/ml (IQR 0.1-29.9) for the PSMA group, respectively. PSMA was positive in 38% of cases: 12% outside of the pelvis and 20% in pelvic lymph nodes. Pre-randomization radiotherapy plan and delivered radiotherapy plan were available in 77/90 control (86%) and 102/103 PSMA (99%) patients (p = 0.0004), respectively. There were 0/77 (0%) and 7/102 (7%) minor changes in the control and PSMA groups (p = 0.02). There were 17/77 (22%) and 46/102 (45%), major changes (p = 0.004), with 33/45 (73%) being PSMA-related:
In another study, Meijer and colleagues assessed whether patients who underwent local salvage radiation therapy after restaging PSMA-PET/CT for biochemical recurrence may have better oncological outcomes than patients who underwent "blind" salvage radiation therapy.5 Among 610 patients who underwent salvage radiation therapy, 298 underwent PSMA PET/CT prior to treatment. After case-control matching, 216 patients were matched in both cohorts (108 patients per cohort). In the patient cohort without PSMA-PET/CT prior to salvage radiation therapy, 23 (21%) had biochemical progression of disease at 1 year after salvage radiation therapy, compared with nine (8%) patients who underwent restaging PSMA-PET/CT prior to salvage radiation therapy (p = 0.007).
Risk grouping and PSMA filters for radiotherapy to the fossa greatly narrows down the patient population that may benefit from treatment for biochemical recurrence: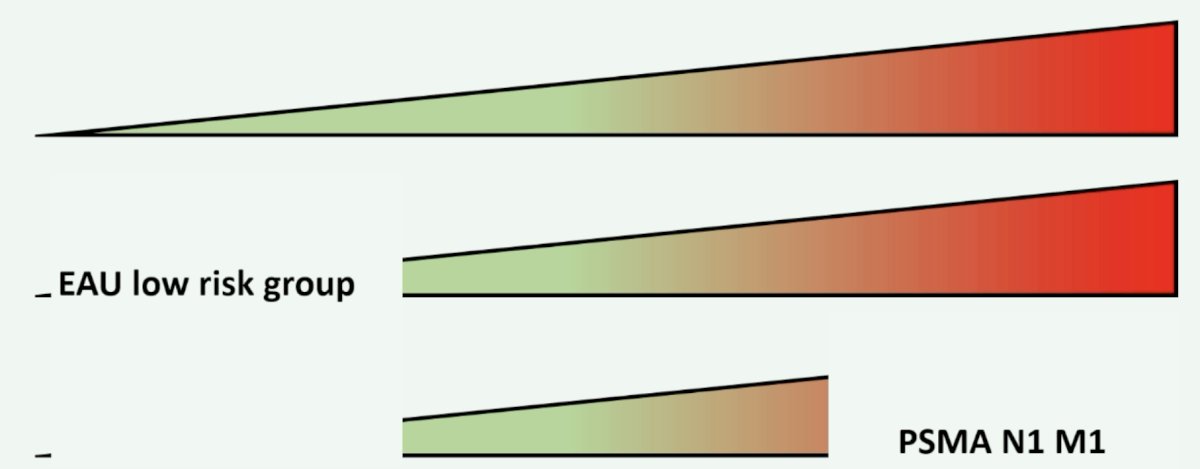
Thus, we are moving from risk-based to imaging-targeted treatment for high-risk biochemical recurrence.
Dr. Van Den Bergh concluded his presentation discussing clinical and molecular stratification of men with biochemical recurrence after radical prostatectomy with the following conclusions:
- Clinical and molecular stratification of men with biochemical recurrence after radical prostatectomy provides information with regards to:
Presented by: Roderick C.N. van den Bergh, St. Antonius Hospital, Utrecht, The Netherlands
Written by: Zachary Klaassen, MD, MSc - Urologic Oncologist, Associate Professor of Urology, Georgia Cancer Center, WellStar MCG Health, @zklaassen_md on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th - April 8th, 2024
References:
- Van Den Broeck T, van den Bergh RCN, Arfi N, et al. Prognostic Value of Biochemical Recurrence Following Treatment with Curative Intent for Prostate Cancer: A Systematic Review. Eur Urol 2019 Jun;75(6):967-987.
- Preisser F, Abrams-Pompe RS, Stelwagen PJ et al. European Association of Urology Biochemical Recurrence Risk Classification as a Decision Tool for Salvage Radiotherapy—A Multicenter Study. Eur Urol. 2024;85:164-170.
- Emmett L, Tang R, Nandurkar R, et al. 3-Year Freedom from Progression After 68Ga-PSMA PET/CT-Triaged Management in Men with Biochemical Recurrence After Radical Prostatectomy: Results of a Prospective Multicenter Trial. J Nucl Med. 2020 Jun;61(6):866-872.
- Armstrong WR, Kishan AU, Booker KM, et al. Impact of Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography on Prostate Cancer Salvage Radiotherapy Management: Results from a Prospective Multicenter Randomized Phase 3 Trial (PSMA-SRT NCT03582774). Eur Urol. 2024 Jan 29 [Epub ahead of print].
- Meijer D, Eppinga WSC, Mohede RM, et al. Prostate-specific Membrane Antigen Positron Emission Tomography/Computed Tomography is Associated with Improved Oncological Outcome in Men Treated with Salvage Radiation Therapy for Biochemically Recurrent Prostate Cancer. Eur Urol Oncol. 2022 Apr;5(2):146-152.


