(UroToday.com) The 2024 European Association of Urology (EAU) annual congress held in Paris, France between April 5th and 8th was host to a joint session of the EAU and the Advanced Prostate Cancer Consensus (APCCC). Professor Aurelius Omlin discussed what to test for prior to the start of hormonal treatment and what to monitor for thereafter.
Professor Omlin noted that the management of mHSPC may be considered a form of tertiary prevention, whereby the aim is to soften the impact of an ongoing illness or injury that has lasting effects. This is done by helping patients manage long-term, often complex health problems in order to improve, as much as possible, their ability to function, their quality of life, and life expectancy.
While there are many considerations for the mHSPC patient, the focus of this discussion will be cardiovascular and bone health aspects.
There appears to be a high cardiovascular disease risk burden in prostate cancer patients. An analysis of RADICAL-PC of 2,711 men published in 2023 demonstrated that 99% of prostate cancer patients had ≥1 uncontrolled cardiovascular risk factor, and 51% had poor overall risk factor control.1 There is clearly a large gap in care and a need for improved interventions to optimize cardiovascular risk management.
Why is controlling cardiovascular disease risk factors important in this setting? Cardiovascular disease is the most common cause of non-prostate cancer related deaths, as demonstrated in a cohort analysis of 26,168 patients with metastatic prostate cancer.2
This risk of cardiovascular disease appears to be further increased in prostate cancer patients receiving ADT. This effect appears to be mediated via hypogonadism-mediated changes, including altered body composition, lipid abnormalities, and impaired glycemic control, as summarized in the flow chart below.

What are the current recommendations from the American Heart Association? Prostate cancer patients receiving ADT should be monitored for cardiovascular disease risk factors, with those at higher risk of metabolic syndrome requiring blood pressuring, serum lipids, body mass index, waist circumference, HbA1c, and fasting blood glucose monitoring (to be performed every 3 months if ≥2 factors are present). A multidisciplinary approach is likely helpful in this setting whereby a cardio-oncology consultation may be considered if patients have pre-existing cardiovascular disease and/or ≥2 risk factors are present, an endocrinology referral if a patient has diabetes, and social work/mental health assistance if there are barriers to care. We note that these recommendations are for patients on ADT. In cases of systemic therapy intensification with ADT + an androgen receptor pathway inhibitor, this risk is further increased, and more vigilant monitoring may be prudent.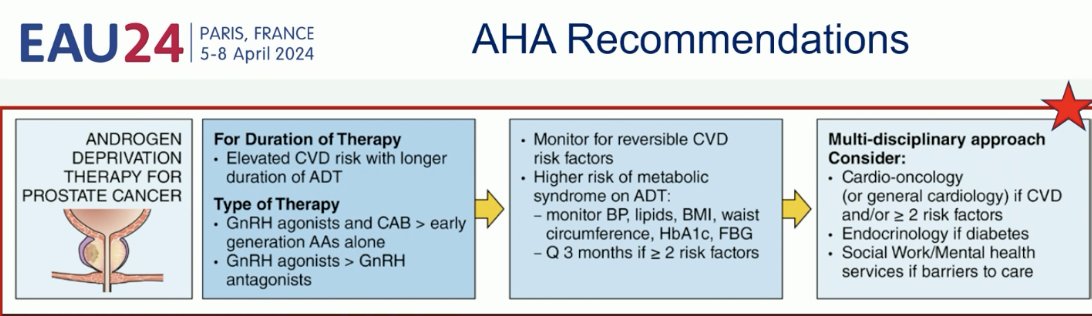
What do the current experts believe is an appropriate work-up prior to the start of hormonal therapy for prostate cancer patients? It appears that the decision-making process is strongly linked to the patient’s underlying risk profile: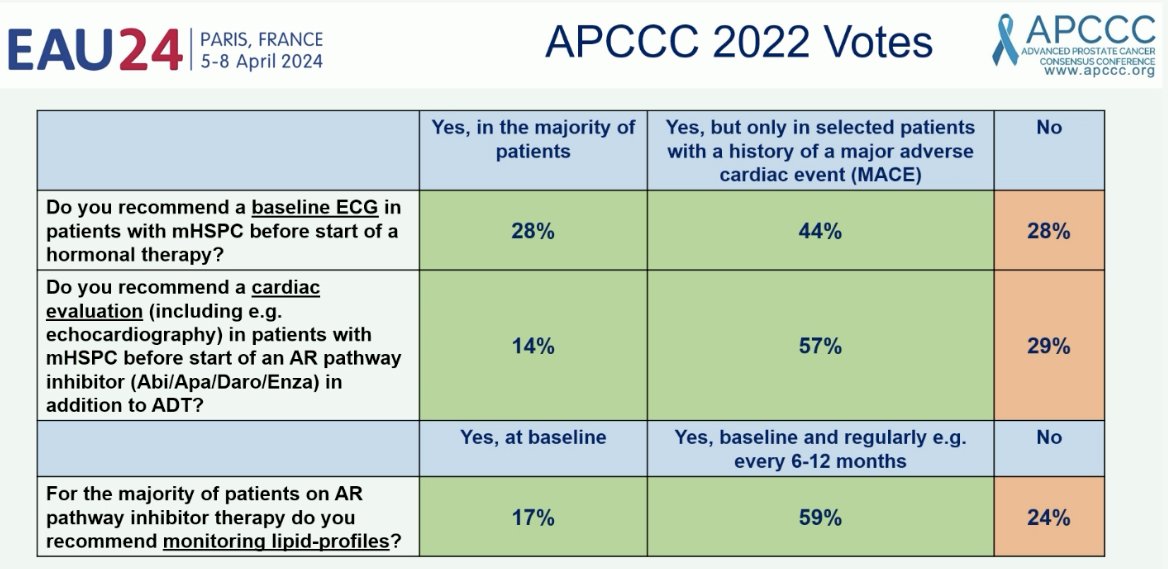
What about bone health? Analysis of the Surveillance, Epidemiology, and End Results (SEER) Medicare program on fracture risk with ADT use in prostate cancer demonstrated that 19.4% of those who received ADT had a fracture, as compared with 12.6% of those not receiving ADT (p<0.001). In the Cox proportional-hazards analyses, adjusted for characteristics of the patient and the tumor, there was a statistically significant association between the number of doses of gonadotropin-releasing hormone received during the 12 months after diagnosis and the subsequent risk of fracture.3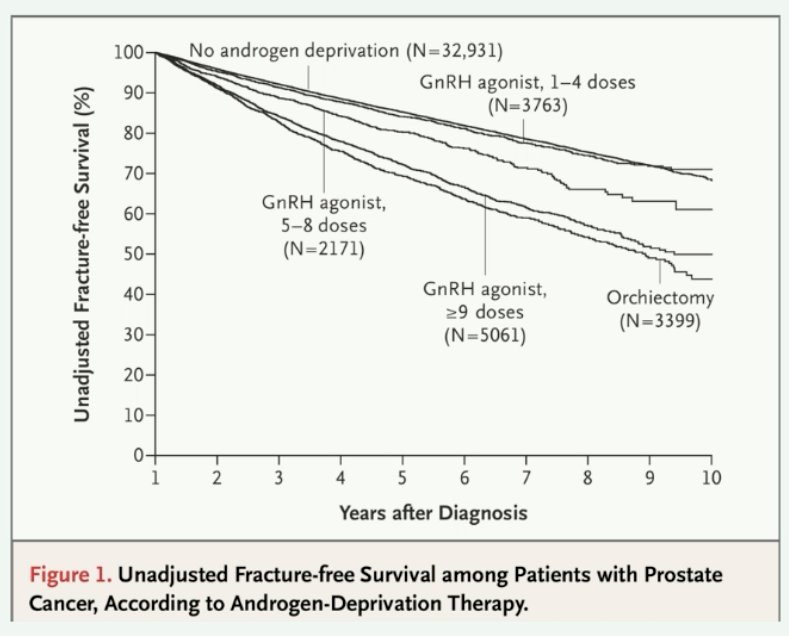
Furthermore, it appears that the addition of an androgen receptor pathway inhibitor to standard ADT significantly increases the risk of fractures and falls in men with prostate cancer enrolled in clinical trials (HR: 2.32, 95% CI: 2.00 – 2.71).4 This risk is likely to be even higher in a real-world setting, given that clinical trials are often biased in favor of improved participant health and performance status.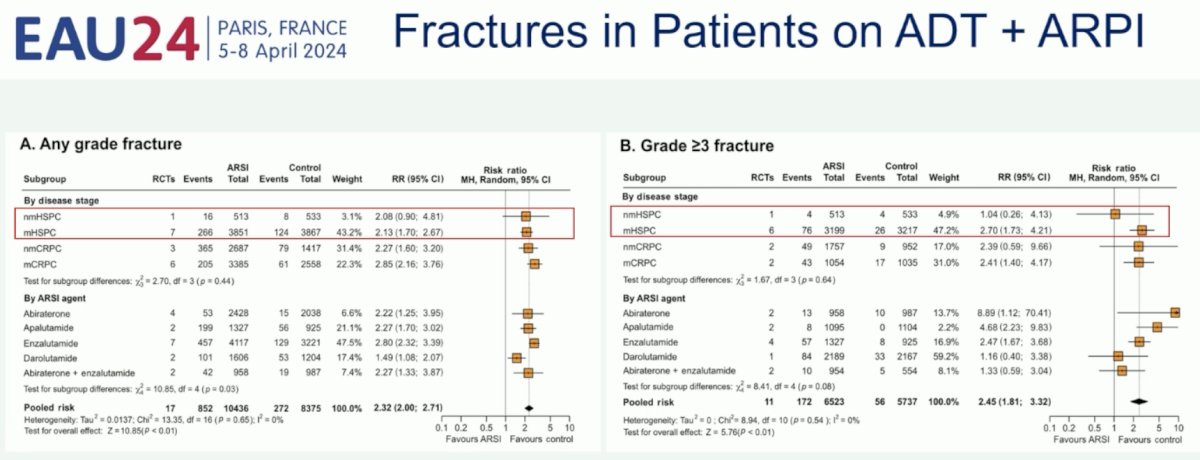
Given this increased risk of bone fractures, there have been concerted efforts by governing bodies to provide clinicians with ‘osteoprotection’ guidelines to address this issue, particularly among patients receiving ‘chronic endocrine treatment known to accelerate bone loss’.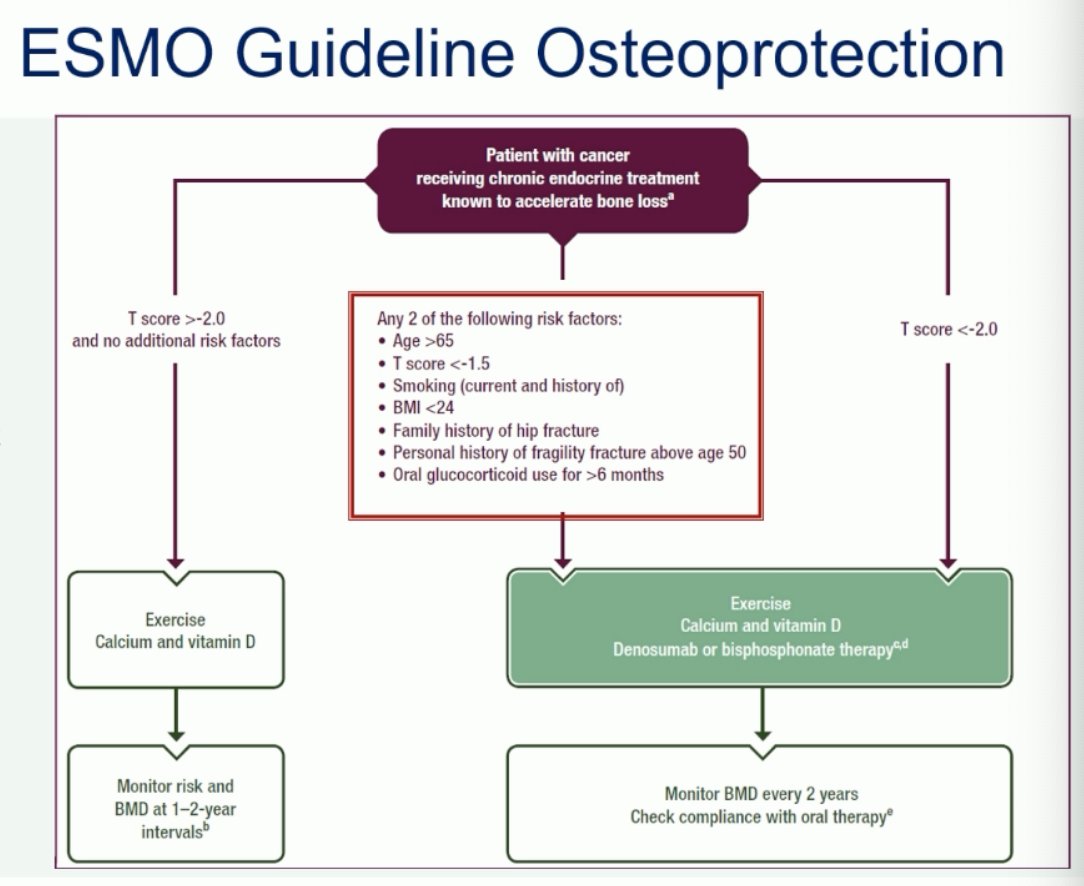
While current guidelines do not recommend the use of bone protective agents routinely in patients with castrate-sensitive disease, the 2022 APCCC survey of experts demonstrated that 63 – 71% would consider denosumab or a bisphosphonate in select patients, as guided by risk assessment scores/guidelines.5
Professor Omlin concluded by acknowledging the recent updates of the 2024 EAU guidelines concurrently published at this meeting, providing nuanced guidance and recommendations on improving bone health in prostate cancer patients receiving hormonal treatment.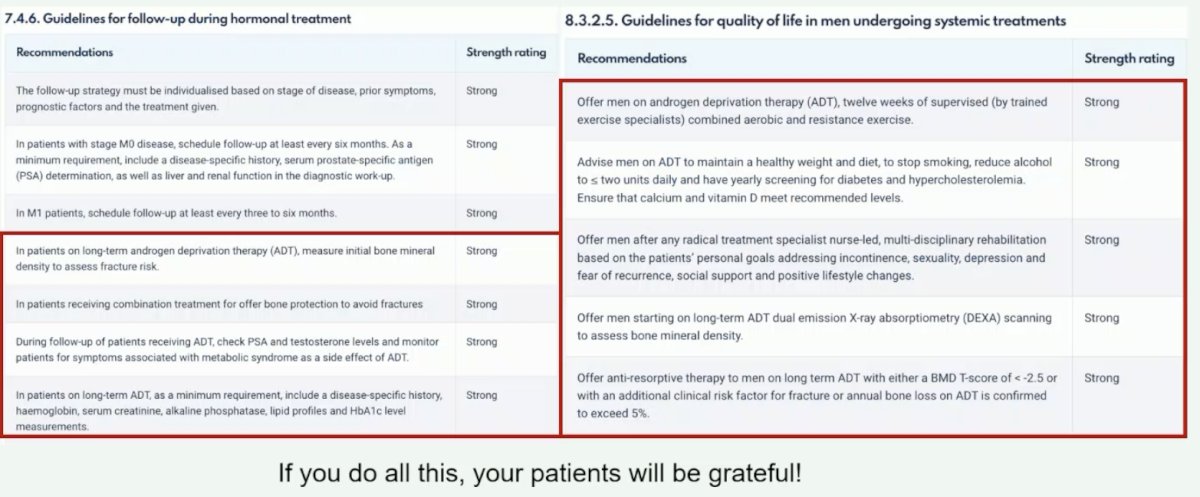
Presented by: Professor Aurelius Omlin, MD, Medical Oncologist at Kantonsspital St. Gallen, Switzerland
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th - April 8th, 2024
References:- Klimis H, Pinthus JH, Aghel N, et al. The Burden of Uncontrolled Cardiovascular Risk Factors in Men With Prostate Cancer: A RADICAL-PC Analysis. JACC CardioOncol. 2023;5(1): 70-81.
- Almehrath AO, Afifi AM, Al-Husseini MJ, et al. Causes of Death Among Patients With Metastatic Prostate Cancer in the US From 2000 to 2016. JAMA Netw Open. 2021;4(8):e2119568.
- Shahinian VB, Kuo Y, Freeman JL, Goodwin JS. Risk of fracture after androgen deprivation for prostate cancer. N Engl J Med. 2005;352(2): 154-64.
- Jones C, Gray S, Brown M, et al. Risk of Fractures and Falls in Men with Advanced or Metastatic Prostate Cancer Receiving Androgen Deprivation Therapy and Treated with Novel Androgen Receptor Signalling Inhibitors: A Systematic Review and Meta-analysis of Randomised Controlled Trials. Eur Urol Oncol. 2024:S2588-9311(24)00042-7.
- Gillessen S, Bossi A, Davis ID, et al. Management of Patients with Advanced Prostate Cancer. Part I: Intermediate-/High-risk and Locally Advanced Disease, Biochemical Relapse, and Side Effects of Hormonal Treatment: Report of the Advanced Prostate Cancer Consensus Conference 2022. Eur Urol. 2023;83(3): 267-293.


