(UroToday.com) The 2024 European Association of Urology (EAU) annual congress held in Paris, France between April 5th and 8th was host to a joint session of the EAU and the Advanced Prostate Cancer Consensus (APCCC). Professor Nick James discussed the optimal treatment in the case of PSA persistence following radical prostatectomy.
Which of these patients should be treated? Professor James argued that this depends on the prior surgical history (i.e., whether prior lymph node dissection was performed and how extensive), surgical pathology, and availability of imaging.
There is some evidence to inform the timing of treatment administration. The RADICALS-RT trial randomized post-prostatectomy patients with a post-operative PSA ≤0.2 ng/ml with ≥1 worrisome clinicopathologic feature to either adjuvant radiotherapy or salvage radiotherapy at the time of PSA failure.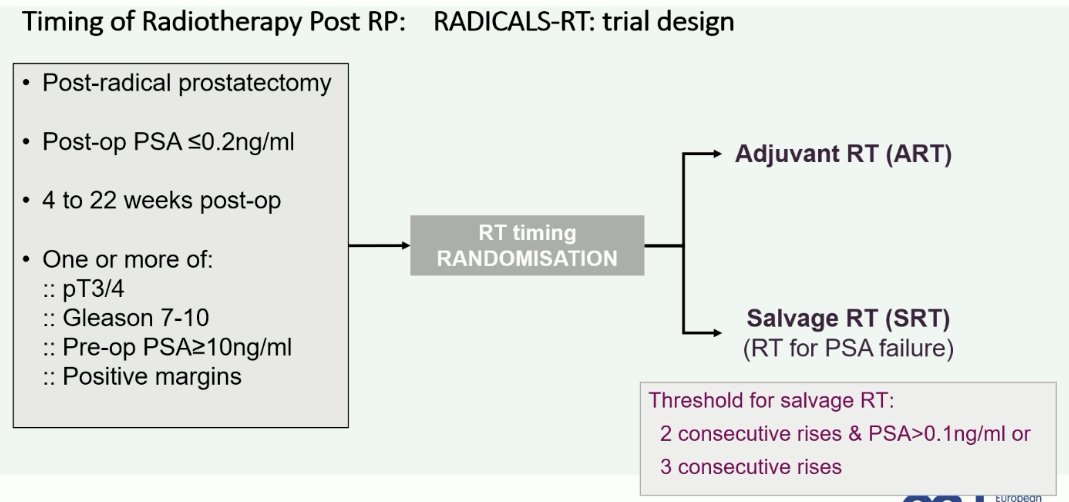
While the RADICALS-RT trial did not necessarily include patients with persistent levels post-operatively, Professor James argued that the results of this trial likely can be generalized to this patient population. As summarized below, the urinary (and bowel) toxicity outcomes are significantly worse for patients who undergo adjuvant radiotherapy, as opposed to salvage radiotherapy.1 As such, Professor James argued that there may be value in delaying radiotherapy in this cohort of patients until there is clear evidence of disease progression.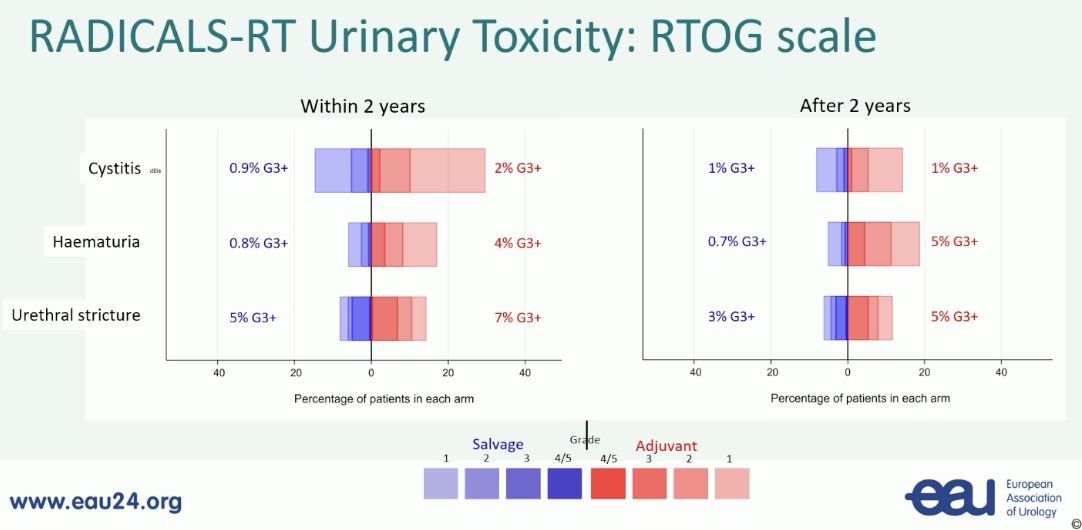
The next question is whether hormone therapy should be added concurrently at time of post-operative radiotherapy. The RADICALS-HD trial evaluated the role of ADT, including duration (6 or 24 months) concurrently with radiotherapy in this setting.
There was no difference in metastasis-free survival among patients who received short-term versus no ADT with post-operative radiotherapy.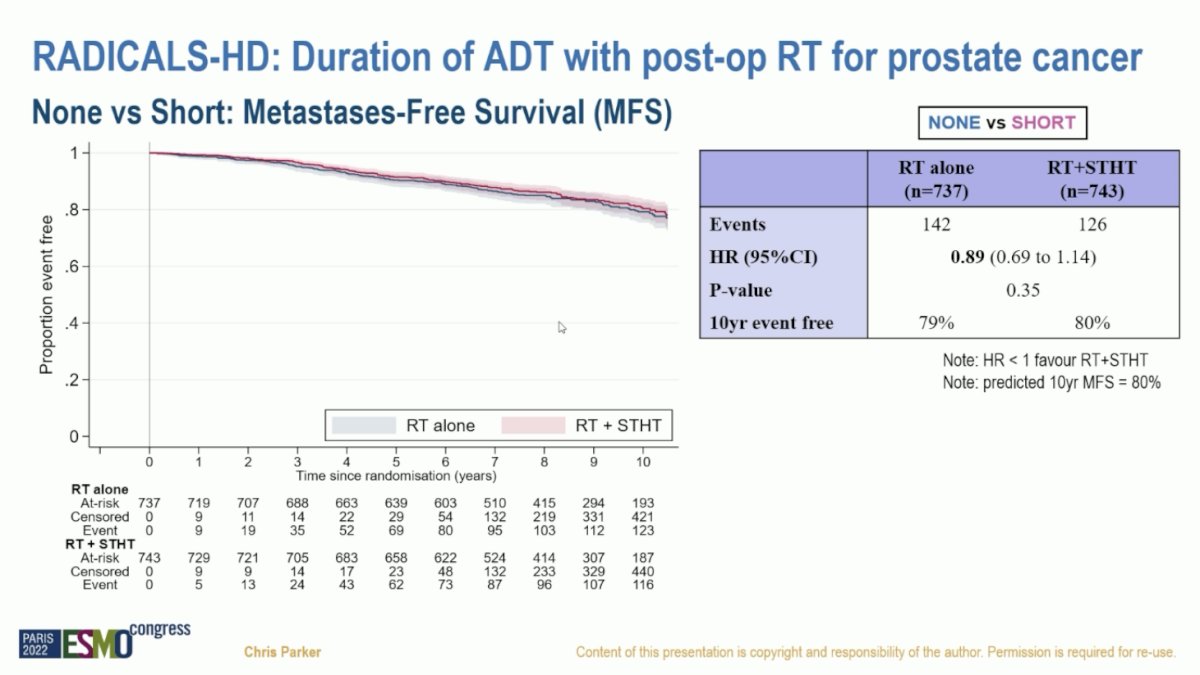
In the second pairwise comparison, patients receiving long-term ADT had significantly superior metastasis-free survival compared to those receiving short-term ADT (HR: 0.77, 95% CI: 0.61–0.97).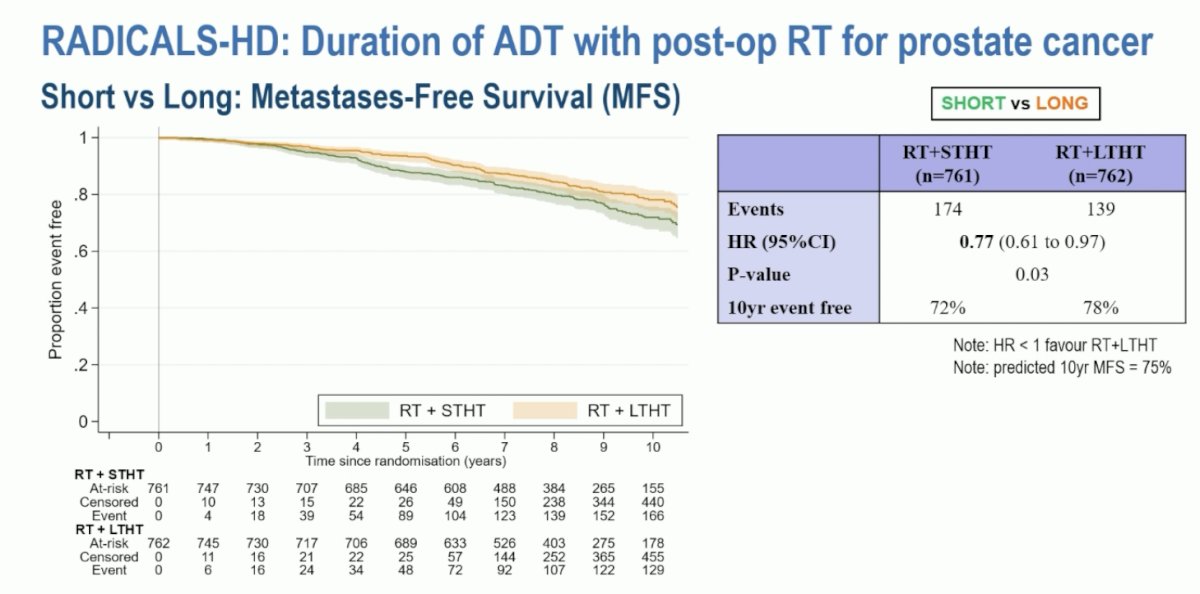
How does prior surgical status, namely relating to prior performance of a lymph node dissection, alter treatment decision making? In patients with no prior node dissection, the morbidity of radiotherapy is likely to be less, but pathologic staging would be less certain. While patients with a prior node dissection are likely to have better pathologic staging, PET data often shows ‘atypical’ relapse patterns/sites.
To date, the extent of nodal dissection has not been demonstrated to significantly impact oncologic outcomes. The randomized clinical trial of extended versus limited nodal dissection failed to reach its primary endpoint of biochemical recurrence-free survival improvement with an extended nodal dissection.2
What about surgical pathology? This information can be used to guide the disease site likelihood in patients with biochemical persistence. If resection margins are clear, then prostatic fossa disease is less likely. Conversely, if resection margins are positive, the opposite scenario becomes more likely. In either case, distant disease cannot be excluded. If patients are node positive and the PSA is still persistently elevated, the disease also remains unpredictable. One thing to note is that as the PSA level rises, the likelihood of PSMA PET imaging detecting the exact site of disease spread/persistence increases.
For patients who undergo adjuvant or salvage radiotherapy post-radical prostatectomy, it is important to note that relapses mainly occur outside the radiotherapy field.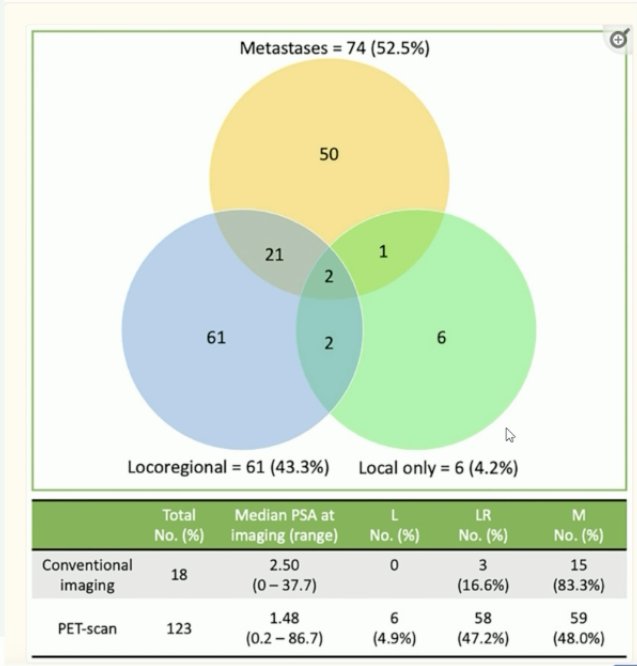
With regards to imaging, PSMA PET is more sensitive than CT, MRI, or bone scan for the detection of nodal relapse. However, at low PSA values (<1 ng/ml), there are significant false-negative rates for pelvic lymph nodes. At higher PSA values, sensitivity improves but is more likely to be low volume M1.
Professor James concluded with the following take home messages regarding PSA persistence and relapse:
- The patterns of relapse are complex and unpredictable.
- The sites of relapse may be influenced by prior surgery, but more extensive surgery is probably best viewed as a staging rather than a therapeutic procedure
- Relapses can occur in the surgical field, but rare inside the radiotherapy field
- The current literature supports more limited surgery and more frequent imaging to best define sites for radiotherapy in the relapse setting
Presented by: Professor Nick James, MBBS, PhD, Professor of Prostate and Bladder Cancer Research at The Institute of Cancer Research and The Royal Marsden NHS Foundation Trust, London, UK
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th - April 8th, 2024
References:- Sargos P, Chabaud S, Latorzeff I, et al. Adjuvant radiotherapy versus early salvage radiotherapy plus short-term androgen deprivation therapy in men with localized prostate cancer after radical prostatectomy (GETUG-AFU 17): A randomized, phase 3 trial. Lancet Oncol 2020;21(10):1341-1352.
- Touijer KA, Sjoberg DD, Benfante N, et al. Limited versus Extended Pelvic Lymph Node Dissection for Prostate Cancer: A Randomized Clinical Trial. Eur Urol Oncol. 2021;4(4): 532-539.


