(UroToday.com) The 2024 European Association of Urology (EAU) annual congress held in Paris, France between April 5th and 8th was host to a plenary session addressing imaging-related controversies for the staging of genitourinary cancers. Drs. Morgan Rouprêt, Sarah Psutka, and Arnulf Stenzl participated in a rapid-fire debate discussing the optimal management of patients with non-invasive, high-grade upper tract disease in the setting of a prior radical cystectomy.
Professor Rouprêt presented a case of a 72-year-old male with gross hematuria, who had previously undergone a radical cystectomy and ileal conduit for cT2N0 urothelial carcinoma of the bladder four years ago. His glomerular filtration rate was 80 mL/min. His CT scan performed for this hematuria demonstrated evidence of a 2 cm tumor in his left kidney, without evidence of local invasion or adenopathy. A flexible ureteroscopy and biopsy was performed demonstrating evidence of high-grade disease.
What is the optimal management of this patient? Would this change if eGFR was 50 ml/min instead of 80 ml/min?
Dr. Psutka noted that there is a clear survival benefit for radical nephroureterectomy, compared to conservative approaches, for the management of patients with high-risk upper tract urothelial carcinoma.1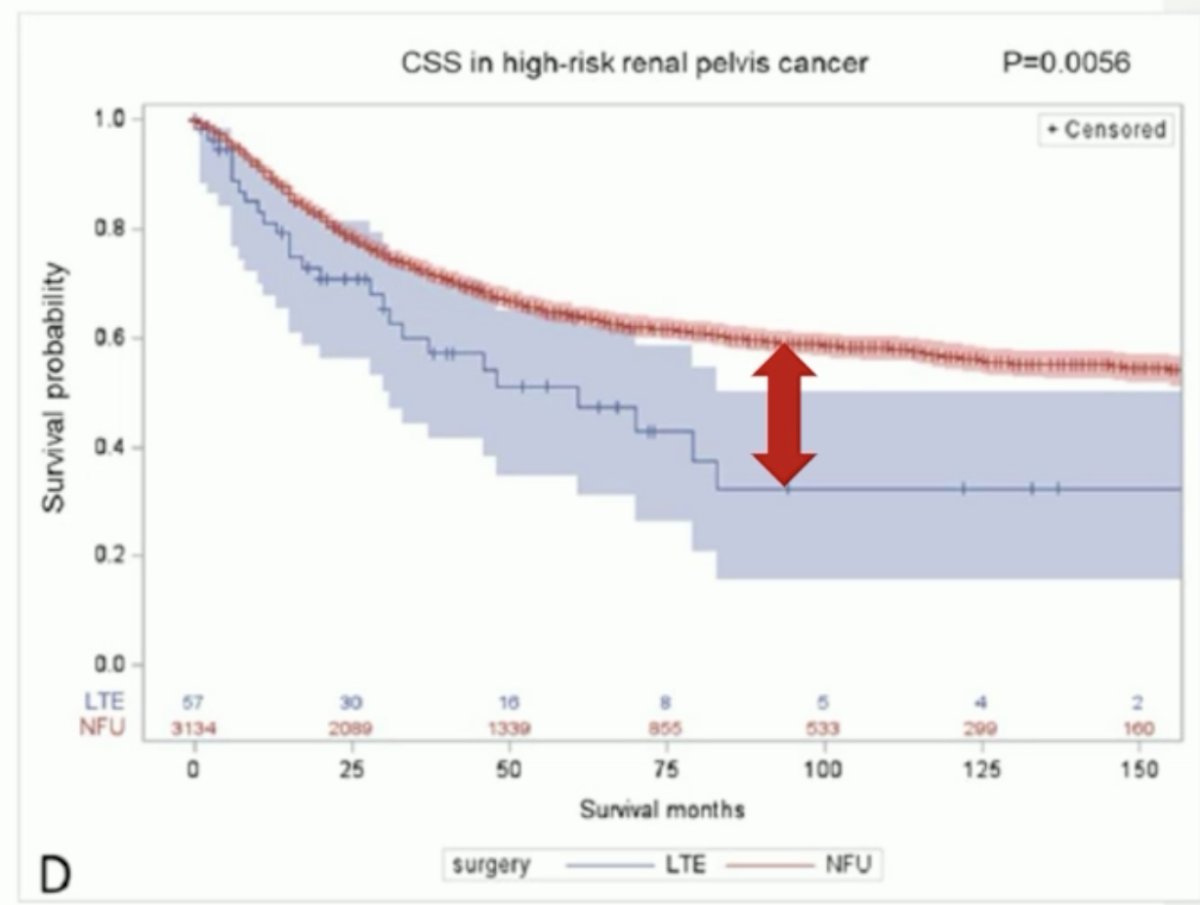
However, in select cases, conservative management is a viable option for patients with high-grade tumors. In a retrospective series of 65 patients (≤pT1: 57%, high grade: 40%) followed for a median of 75 months, the long-term cancer specific survival was 92%.2 Although these results are promising, they do highlight the importance of patient counseling and stringent follow-up with routine cystoscopies and a second look ureteroscopy at 6–8 weeks following treatment.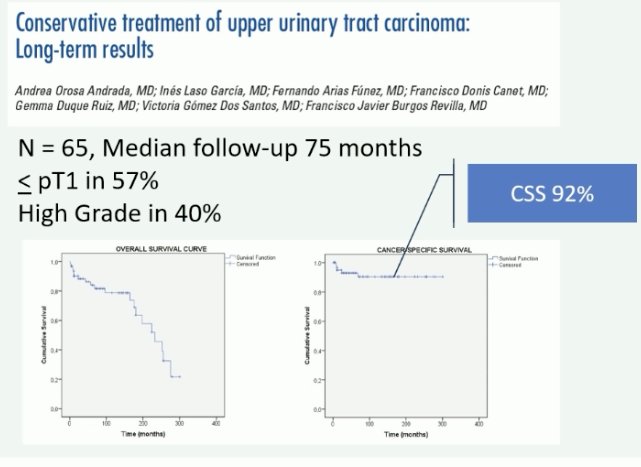
Should conservative therapy options be offered to the patient presented earlier? This patient with a 2 cm upper tract calyceal tumor has an expected life expectancy of ~13 years, with a 5-year mortality rate ranging between 13% and 70%, depending on his comorbidity status.
What do the guidelines tell us in this situation? This patient meets the criteria for AUA favorable high-risk disease. Tumor ablation may be the initial management option offered to select patients with high-risk favorable disease who have low-volume tumors or cannot undergo a radical nephroureterectomy (Conditional Recommendation; Evidence Level: Grade C).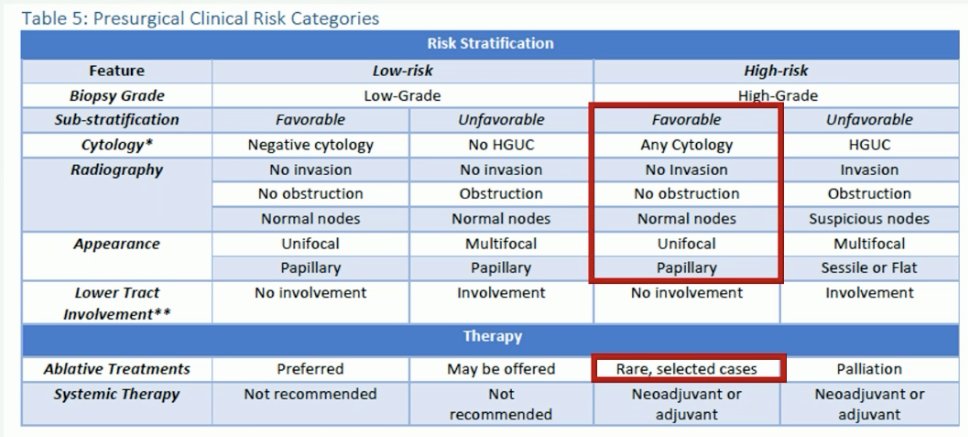
The EAU supports a similar approach to these patients with kidney-sparing management considered a reasonable approach for high-risk patients with ‘imperative’ indications.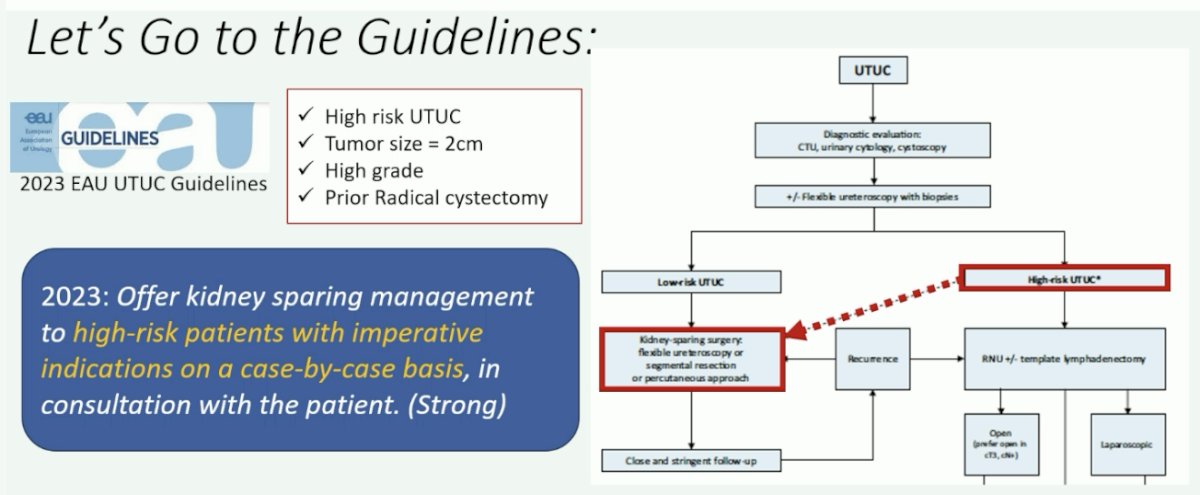
Imperative indications for kidney sparing approaches include:
- Solitary kidney
- Presence of bilateral upper tract disease
- Of note, this patient has a history of muscle invasive bladder cancer and, as such, his risk of contralateral upper tract disease is 0.6–7%
- Comorbidity burden prohibiting radical nephroureterectomy
- Chronic kidney disease
We also cannot underestimate the surgical morbidity of a radical nephroureterectomy in a patient with a prior radical cystectomy/ileal conduit. There is a high likelihood of needing an extensive lysis of adhesions, post-operative ileus, small bowel obstruction, risk of compromising the vascular supply to the ileal conduit, disrupting the ureteral-enteric anastomosis, urine leak, and bowel injury. This is reflected by the output from the ACS (American College of Surgeons) risk calculator demonstrating that this patient’s risk of any complication in the 90-day post-radical nephroureterectomy period is as high as 40%.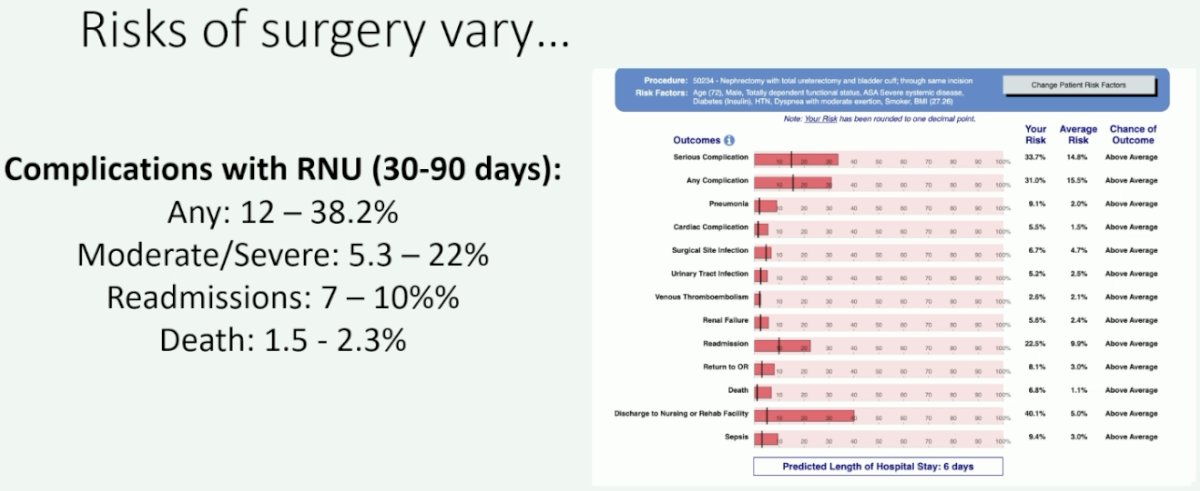
We also cannot underestimate the impact of major surgical interventions on cognition, with studies suggesting that post-operative delirium in such elderly patients is as high as 60% and anesthesia-related cognitive decline occurs in one of three such patients. It is also important to note that among older adults with cancer, >70% would not choose a treatment to extend their survival if it were expected to cause severe functional impairment.
What do we know about kidney function following radical cystectomy? Kidney function declines by 2.1% per year following radical cystectomy with ileal conduit. Furthermore, kidney function declines by 24% following a radical nephroureterectomy. As such, a radical nephroureterectomy in patients with prior radical cystectomy are at particularly high risk of renal function decline.
Dr. Psutka concluded by noting that this patient should be offered a conservative, kidney-sparing approach, given its concordance with current guidelines recommendations, the potential to avoid CKD in a patient at risk of accelerated renal function decline, maintain options in the event of a future contralateral upper tract occurrence, and avoid exposure to the surgical risks of radical nephroureterectomy, with acceptable expected oncologic efficacy. In this setting, we must acknowledge the increased risk of disease progression with a conservative approach, implement rigorous surveillance, and proactively discuss anticipated salvage treatment options.
Next, Professor Stenzl argued in favor of radical nephroureterectomy. This patient meets the criteria for high-risk upper tract disease given his tumor size ≥2 cm with evidence of high-grade disease on cytology and ureteroscopic biopsy.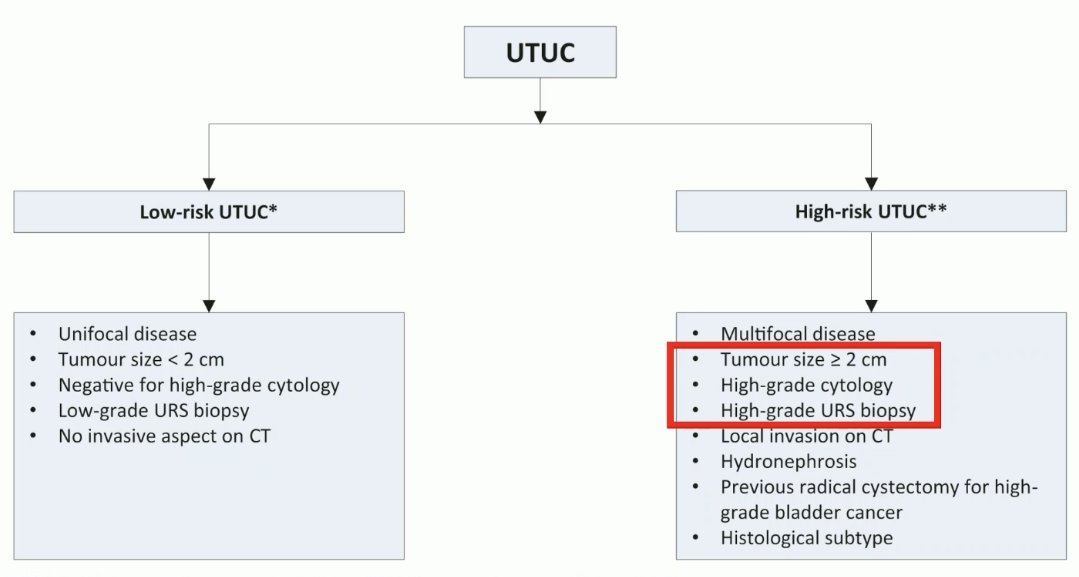
Per the current EAU guidelines, it is recommended that this patient undergo a radical nephroureterectomy, with conservative therapy a secondary consideration in this patient.
Another important aspect is that high-risk patients undergoing a radical nephroureterectomy should be considered for a concurrent lymphadenectomy, with the template varying by the tumor location.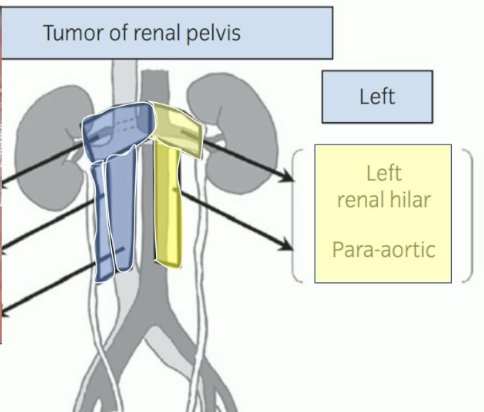
What if the patient has an eGFR of <50 ml/min? In these patients, kidney-sparing approaches may be considered with endoscopic resection using rigid ureteroscopes and laser ablation using flexible ureteroscopes. However, there are significant technical challenges associated with these approaches.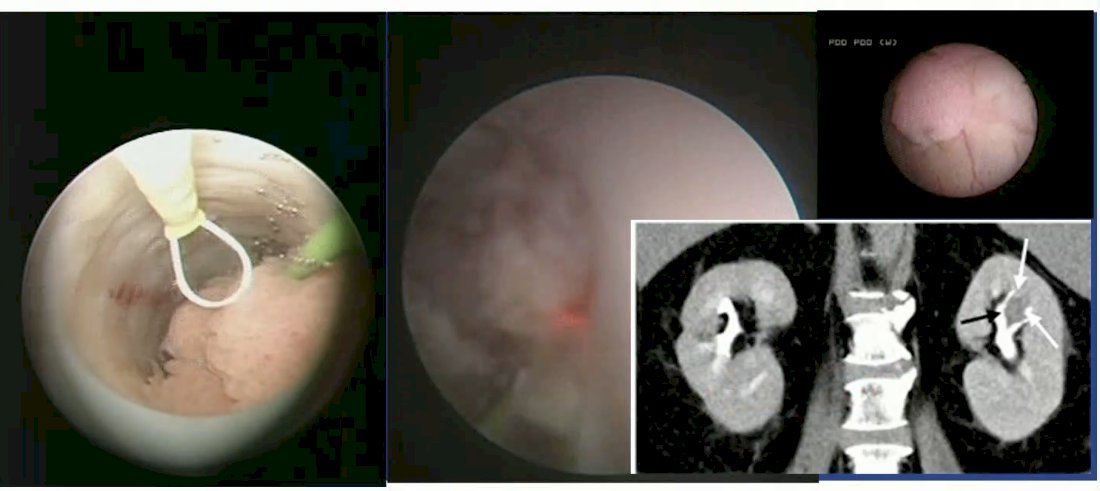
Additional challenges associated with the adoption of conservative strategies include those relating to the instillation of adjuvant therapies, including mitomycin and BCG, which may require retrograde instillation via a ureter catheter or antegrade percutaneous access, with such a decision related to the site of disease and the patient’s anatomy. Furthermore, there is a lack of robust data supporting such practices in this rare, often heterogeneous disease process, with the current evidence relying on small, retrospective series and extrapolation from the bladder cancer disease space.
Professor Stenzl concluded that in this patient with high-grade urothelial carcinoma, who had received prior neoadjuvant chemotherapy, has a tumor burden ≥2 cm, a GFR ≥60 ml/min, and a life expectancy of ≥5 years, the standard of care approach should be radical nephroureterectomy +/- lymphadenectomy +/- systemic therapy.
Presented by:
- Professor Morgan Rouprêt, MD, PhD, Department of Urology, Pitié-Salpétrière Hospital, Paris, France
- Sarah Psutka, MD, MSc, Associate Professor, Department of Urology, University of Washington, Seattle, WA
- Professor Arnulf Stenzl, MD, Chairman, Department of Urology, University of Tubingen, Tubingen, Germany
Written by: Rashid Sayyid, MD, MSc - Society of Urologic Oncology (SUO) Clinical Fellow at The University of Toronto, @rksayyid on Twitter during the 2024 European Association of Urology (EAU) annual congress, Paris, France, April 5th - April 8th, 2024
References:- Slusarczyk,A, Zapala P, Zapala L, et al. Oncologic outcomes of patients treated with kidney-sparing surgery or radical nephroureterectomy for upper urinary tract urothelial cancer: a population-based study. Urol Oncol. 2024;42(1): 22.e1-22.e11.
- Andrada AO, Garcia IL, Funez FA, et al. Conservative treatment of upper urinary tract carcinoma: Long-term results. Can Urol Assoc J. 2017;11(7): E291-E296.


