For this study, the development cohort comprised 3,539 prospectively recruited patients recruited at 40 UK hospitals and a validation cohort comprised 656 Swiss patients. All patients were aged >18 years and referred to the hospital for the evaluation of visible and non-visible hematuria. Sensitivity and specificity of the hematuria cancer risk score in the validation cohort were derived from a cut-off identified from the discovery cohort.
The key variables for developing the hematuria cancer risk score included patient age, gender, type of hematuria, and smoking history. The hematuria cancer risk score validation achieved good discrimination (AUC 0.835; 95%CI 0.789-0.880) and calibration (slope=1.215) with no significant overfitting (p=0.151). As follows are the hematuria cancer risk score cutoffs with the associated sensitivity, specificity, true positive and negative and false positive and negative values derived from the ROC curve in the development and validation cohorts:
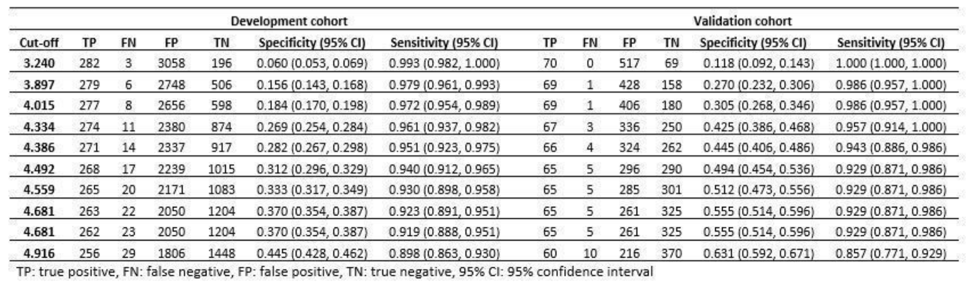
The hematuria cancer risk score detected 11.4% (n=8) more cancers which would have been missed by the UK National Institute for Health and Clinical Excellence guidelines. The American Urological Association guidelines would have identified all cancers with a specificity of 12.6% compared to 30.5% achieved by the hematuria cancer risk score. Of note, based on the hematuria cancer risk score, all patients with upper tract cancers would have been identified. Indeed, this is a potentially useful tool to help guide clinicians as to who should receive a full hematuria workup based on their risk of an underlying malignancy. Certainly, with further validation, the hematuria cancer risk score may become mainstream in primary care and urology clinics.
The authors concluded that the hematuria cancer risk score offers good discriminatory accuracy, which is superior to existing guidelines. The simplicity of the model would facilitate adoption and improve patient and physician decision making.
Presented by: Wei Shen Tan, MBBCh BSc MRCS, the University College London, Department of Urology, London, United Kingdom
Written by: Zachary Klaassen, MD, MSc – Assistant Professor of Urology, Georgia Cancer Center, Augusta University - Medical College of Georgia, Twitter: @zklaassen_md at the 34th European Association of Urology (EAU 2019) #EAU19 conference in Barcelona, Spain, March 15-19, 2019.
References:
1. Nielsen M, Qaseem A, High Value Care Task Force of the American College of Physicians. Hematuria as a Marker of Occult Urinary Tract Cancer: Advice for High-Value Care From the American College of Physicians. Ann Intern Med. 2016 Apr 5;164(7):488–497.


