Barcelona, Spain (UroToday.com) Active Surveillance (AS) for prostate cancer (PCa) is the standard of care of men with low-risk PCa. However, approximately 30-40% of men on AS will eventually progress to treatment – either due to choice or due to progression. Progression can either be due to grade or volume progression, on individual biopsies. Yet, the strength of AS has often been the belief and expectation that when progressing to treatment, the pathology will not be adversely affected by delaying therapy. Prior prospective trials have reported on this with promising results. In this study, the authors add to the literature and correlate the time on AS to final pathology and oncologic outcomes in men undergoing radical prostatectomy (RP) as definitive therapy.
The authors utilized a prospectively maintained AS database at Princess Margaret Cancer Centre and specifically identified men on AS who progressed to RP (n=294) between 1992-2015. Patients undergoing RP for clinically significant PCa were selected (ASRP, n=170). Clinical and pathological characteristics at time of progression to RP (age, PSA, year of biopsy, Gleason score and primary Gleason grade) were used to compare pathologic and oncologic outcomes to a matched cohort (1:4 matching) of patients treated with upfront RP at diagnosis (n=405) – matched based on age, year of final biopsy, clinical stage, Gleason Score and PSA. The main outcomes were biochemical recurrence (BCR) free survival, cancer-specific survival (CSS) and overall survival (OS).
Of the 170 men on AS who underwent RP for clinical significant PCa (grade progression or volume progression), the median time on AS was 31.0 months (Interquartile range (IQR): 30.0-44.0), or approximately 2.5 years. Summary of demographics and comparison of the two groups are seen below: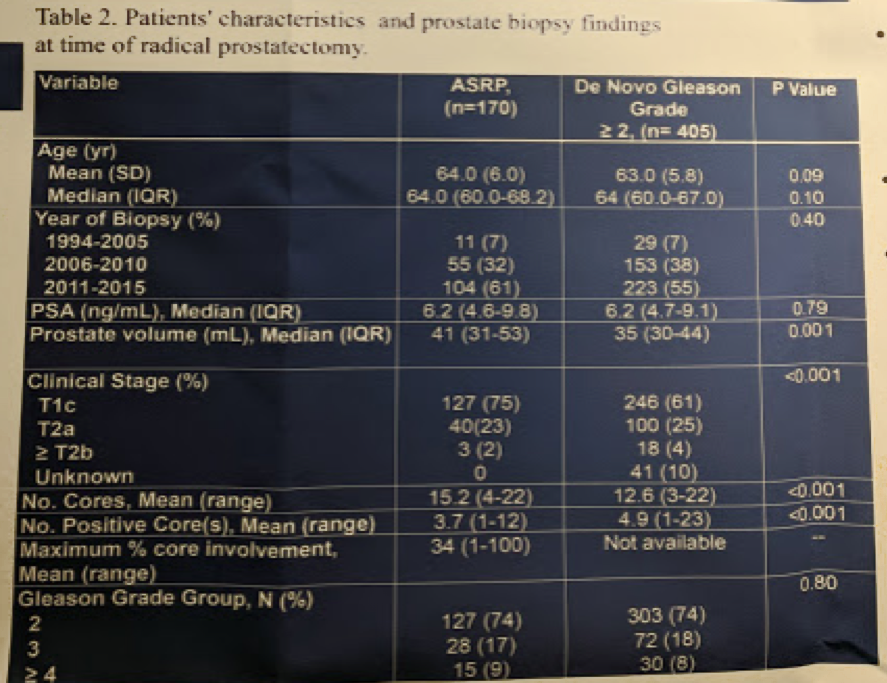
At the time RP, the rate of adverse pathologic features, including pT3, pN1 and positive surgical margin rate (PSM) were comparable between the ASRP group and matched controls. When comparing the two groups, the ASRP cohort had a smaller cancer volume. They were also more likely to undergo nerve-sparing at the time of RP. Pathologic comparisons are below: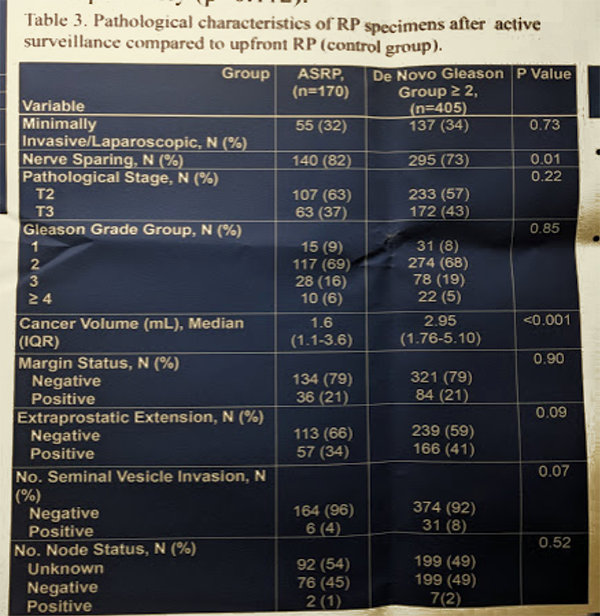
In terms of oncologic outcomes, median follow-up after RP was 5.6 years for both cohorts. At 5 years the BCR free survival rate in ASRP cohort and upfront RP cohort were 85.8% and 82.4%, respectively (p=0.112). Oncologic outcomes are summarized below:
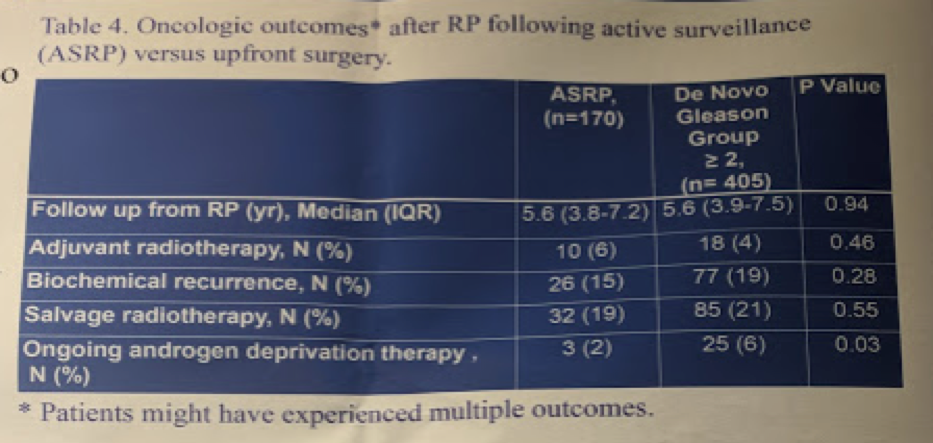
Of note, ADT was used more often in the upfront RP cohort.
BCR-free survival is demonstrated below: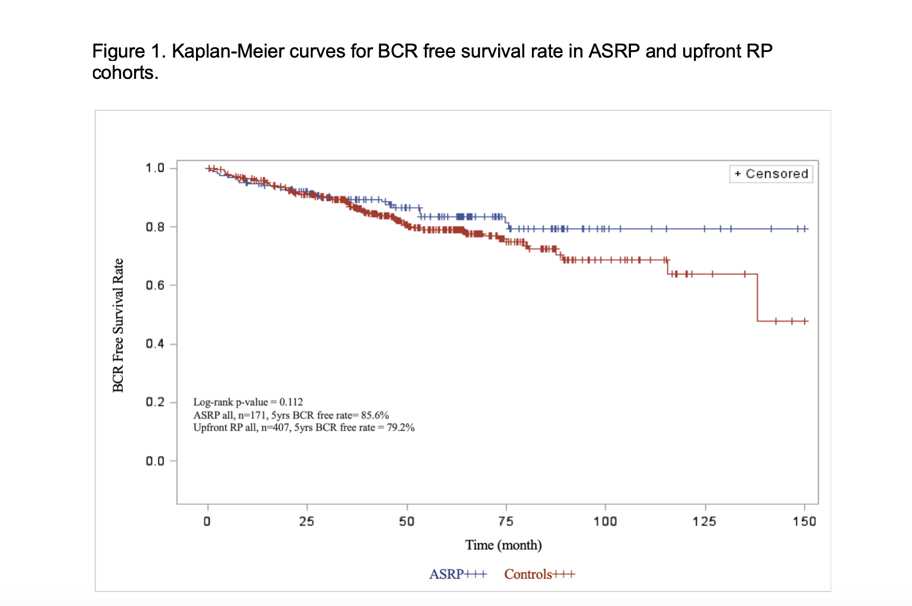
There is no significant difference at 5-years – though perhaps a separation later in the curves.
In terms of CSS, one patient in the ASRP and 6 in the upfront RP cohort died of PCa. 5-year CSS was 100% and 99.7% (no significant difference). 5-year OS was 98.1% and 99.7% (no significant difference).
Based on this single institution experience over many years, it would appear that despite 2.5 years (median) on AS, the final pathology and oncologic outcomes of men undergoing RP were no different than men who received upfront RP. More importantly, they were not worse. Obviously, there are inherent selection biases in this retrospective study. But, this study does reassure us that waiting on AS does not result in suddenly advanced disease or significantly worse pathology.
Presented by: Ardalan Ahmad, MD, FRCSC, GU Oncologist, Princess Margaret Cancer Centre, University Health Network, University of Toronto, Department of Surgical Oncology, Division of Urology, Toronto, Canada
Written by: Thenappan Chandrasekar, MD (Clinical Instructor, Thomas Jefferson University) (twitter: @tchandra_uromd, @TjuUrology) at the 34th European Association of Urology (EAU 2019) #EAU19, conference in Barcelona, Spain from March 15-19, 2019.


